
Topics
Guests
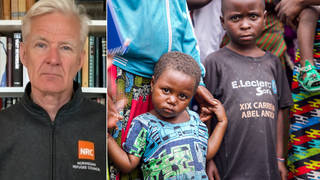
- Stacie Rittermother of twin daughters with cancer. CIGNA denied covering growth hormone treatment for the daughters last year.
Stacie Ritter’s twin daughters were diagnosed with cancer at the age of four. Their insurance provider, CIGNA, denied them coverage even though they had been covered by the family’s former insurer. The incident marked just the latest chapter in the family’s ongoing troubles with the health insurance industry. A few years ago, the Ritters filed for bankruptcy due to their high medical expenses — even though they had health insurance at the time. Stacie Ritter joins us to tell her story. [includes rush transcript]
Transcript
JUAN GONZALEZ: Thousands of patients and healthcare reform activists have been staging protests in recent weeks outside the offices of the nation’s major health insurance companies. In New York, seventeen people were arrested Monday outside the office of Aetna. In Chicago, six people were arrested last week outside the downtown headquarters of Blue Cross and Blue Shield of Illinois.
Our next guest took part in a protest last week outside the corporate headquarters of CIGNA in Philadelphia, where she shared her story about how CIGNA had denied medical care for her family. Stacie Ritter has twin daughters, Madeline and Hannah, who were diagnosed with cancer at the age of four. Last year, CIGNA refused to cover growth hormone therapy for Madeline and Hannah, and even though it was prescribed by their endocrinologist, had been previously covered by the family’s former insurer.
AMY GOODMAN: For months, Stacie Ritter fought with CIGNA, but the company refused to reverse its decision.
The incident marked just the latest chapter in the family’s ongoing troubles with the health insurance industry. A few years ago, the Ritters filed for bankruptcy due to their high medical expenses, even though they had health insurance at the time.
Well, to talk more about what happened, Stacie Ritter joins us now from a studio in Philadelphia. We did invite CIGNA to join as well, but the company declined our request. Stacie Ritter joins us now.
Welcome to Democracy Now!
STACIE RITTER: Hi. Thank you, Amy. Thanks for having me.
AMY GOODMAN: Hi, Stacie. Tell us your story.
STACIE RITTER: Well, it’s a rather long one, so I’ll try to make it as brief as I can.
Our issues with insurance companies have been going on now for quite a while. It didn’t start with CIGNA, though, until April Fool’s Day of 2008. That’s when my husband’s employer switched insurers to CIGNA, which, again, as far as healthcare is concerned, you don’t have a choice. When your employer switches insurers, you get what they give you. And unfortunately, we were given CIGNA.
My girls are cancer survivors. They had pituitary and hypothalamus gland damage as a result of chemo and total body radiation to treat their cancer as part of the stem cell transplant that they had when they were four years old. And a lot of times when a child has that issue, they end up on growth hormone. Many years later, once the oncologist notices a — like a plateau in their growth, which mine did back in 2005, so she referred us to an endocrinologist at Children’s Hospital in Philadelphia, and he monitored them. And they didn’t start growth hormone until 2007. So that was two years of monitoring to make sure, you know, that it wasn’t just a little lax in their growth and that it was really a damaged pituitary and hypothalamus.
And once they started the growth hormone under our previous insurer, which was Aetna, they did very, very well. And so, our doctors said, well, then, that’s — their positive response to the medication is proof that it was damaged, then, the hypothalamus and the pituitary gland. So that was great, so we’ll continue to do this until their bones start to fuse and they no longer need growth hormone.
But unfortunately, CIGNA does not feel the same way that our previous insurer and our world-renowned expert doctor felt. So they claim to have had two endocrinologists look at our case, and both of their endocrinologists deemed that my girls just suffer from idiopathic short stature, which means short stature of unknown origin. But quite to the contrary, we know the origin. We have lots of documentation and proof of the origin.
AMY GOODMAN: And that was — you say that was the radiation that they were exposed to to deal with their rare cancer.
STACIE RITTER: Yes. And chemotherapies, too, are very toxic, and also depends on the child’s age at the time, and even the sex has a lot to do with it. So, the younger the child, especially under five, which mine were — they were four at the time — and the sex — females tend to suffer more damage than males for some reason from the total body radiation. Not all children with cancer have these kind of late-term effects. It’s only children who have had radiation to the brain area, which mine did.
JUAN GONZALEZ: Well, and once CIGNA denied you, how long did the appeals process go on for you to try to get them to reverse the decision? And what was happening in between the time that they denied you? Did they immediately — were your daughters then not able to get the drug?
STACIE RITTER: Well, we were very fortunate to be treated at Children’s Hospital. The doctors there know how the insurance companies work. So when I told them ahead of time that my husband’s employer was switching insurers, they immediately enrolled us in a program sponsored by the drug company that makes the growth hormone that we’re using. And that program is like a bridge program, where they will supply and even have representatives represent me in the appeals process. So, no, we didn’t have to go without it, thankfully, because my doctors were proactive and knew that the insurance company was going to go through this and deny it and give us the runaround.
Once — it was about three months of dealing with CIGNA. My doctors called them and did a peer-to-peer, because they were not approving it. The written information and the medical documents were not enough for CIGNA, so they had a peer-to-peer review scheduled. And CIGNA even went as far as approving the medication for my one daughter on that peer-to-peer review with our endocrinologist and claiming that it had no knowledge of my other daughter existing. They had the knowledge that she existed when they sent me the denials for her.
AMY GOODMAN: They’re identical twins.
STACIE RITTER: Yes, mm-hmm.
AMY GOODMAN: Well, we invited CIGNA to join us on the program, but the company declined our request. The spokesperson, Chris Curran, issued the following statement, quote, “There was no laboratory evidence of growth hormone deficiency. Over a year ago, we had two endocrinologists review this case and based on the laboratory studies, they agreed there is no need for the drug. This is the first time we are hearing about the family’s concerns and disagreement with the decision. We would welcome review of new information as technology and medical evidence is in constant evolution.” Your response, Stacie Ritter?
STACIE RITTER: That’s a joke. Actually, I just received — every year we have to re-enroll in this program. And my doctor had to resubmit a request for coverage to CIGNA again this year. And we just received this year’s denial letters from CIGNA on the situation and then had to re-enroll again with the manufacturer. And that’s carrying us through then. So they are very aware of this situation. They have been.
Unfortunately, our primary endocrinologist who was handling our case had passed away himself of pancreatic cancer last year. And in the scurry to try to cover all of his patients, you know, all of the doctors there in the endocrinology department have had to divide them up. So I’ve had at least four different endocrinologists from CHOP working on my case alone, from writing letters to the peer-to-peer, to the correspondence from the manufacturer, to me calling them. They’re very aware of the situation.
JUAN GONZALEZ: Well, I’d like to turn for a moment to a former CIGNA executive, Wendell Potter, who we’ve interviewed on Democracy Now! in the past. Up until this year, Potter was head of communications for CIGNA, and since leaving the company, he’s become a prominent critic of the health insurance industry. Wendell Potter accused CIGNA of dumping the sick to maximize its profit.
WENDELL POTTER: They have begun shifting their business model away from managed care, which, frankly, I used to think was a great model, a great concept, for the delivery of healthcare. But they’ve moved — they’re moving away from that to what they refer to as consumer-driven or consumer-directed care, and it really is just a euphemism for shifting the financial burden from insurers and employers onto the shoulders of working men and women. I saw that happening. But I also saw how — you know, the things that they do to maximize their profit, which really boils down to dumping the sick.
AMY GOODMAN: What do you mean, “dumping the sick”?
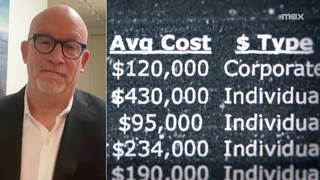
WENDELL POTTER: Two different ways that they do this. In the individual insurance market, we’ve seen quite a bit of news coverage, especially in California. When insurance companies who are active in the individual market — and this means when you don’t get your insurance coverage through your workplace, about the only option you have is to buy it directly from an insurance company, and usually it’s much more costly than it is through — if you buy it or get it through your employer. Once you file a claim, if you are unfortunate enough to get very sick or have an accident and file a claim, you very often will find that your insurance company will go back and look at your application to see if there might be a chance that you either didn’t disclose something that you knew about in the past or inadvertently didn’t disclose something or might not have known about a pre-existing condition. They’ll use that as evidence that you were committing fraud, and they’ll revoke your policy, or they call it “rescinding” your policy, leaving you holding the bag, making you completely responsible for all the medical bills. That’s one way that they dump people who need insurance the most.
Another is, if you are employed, particularly with a small business, and your insurance — your employer gets his or her insurance through one of the large insurers, and if just one person in your company files a claim that the underwriters think is too high, if it skews what they think is the appropriate medical experience or claim experience, when that business comes up for renewal, they very likely will jack up the rates so much that your employer has no alternative but to leave and leave you and all of your coworkers without insurance. Either that or they may cut benefits or try to shop for coverage somewhere else. But the end result is, you may find yourself dumped into the rolls and the ranks of the uninsured.
AMY GOODMAN: And this is a man who knows. Wendell Potter is a whistleblower. He was the corporate spokesperson for CIGNA, actually all through the time, Stacie Ritter, that you were applying and been denied by CIGNA. But he wouldn’t have dealt with this case unless you had gone public, and you’ve only chose to go public now. Why now?
STACIE RITTER: Well, when you’re going through this, and you’re in the day-to-day, you do everything you can to get through the day. It took me six years after the girls’ treatment to actually be able to go out and help work towards securing funding and stuff for research for childhood cancer. It takes a while for a family who is being affected by medical problems to have the opportunity to leave their family for a little while to go try to help fix the situation.
That’s another thing that makes this so sad, is that they have people at such a huge disadvantage, because when you’re going through and you’ve got cancer or your child has cancer, you just want to make sure that your family is still here tomorrow. So you let these people walk on you for the time being, because they’re not your priority. It’s not ’til the aftermath of everything. It was a year after the girls were out of transplant that we filed for bankruptcy. I think nobody has time to deal with that when they’re sick.
AMY GOODMAN: You filed for bankruptcy when, actually, you were getting Aetna insurance, right, and they were approving the coverage?
STACIE RITTER: Correct, yeah. We actually started out with pretty decent coverage from Aetna, initially, when Aetna used to be Aetna US Healthcare. And then Aetna and US Healthcare somehow split and became just Aetna Corporation. And it all went downhill from there, as far as Aetna is concerned.
But when you’re talking premiums, things that aren’t covered, caps on your coverage, deductibles, you’ve got co-pays, you’ve got different prices that you pay for different medicines and the different formularies, then they nickel and dime you to death, and it all adds up.
And when your husband — you know, my husband had to stop working, because I was pregnant at the time, and we had a one-year-old. And between going back and forth from the hospital and somebody watching our son, we really didn’t have another, you know, option than for him to stop working. So we had no real income coming in. And we were paying COBRA payments in order to maintain our insurance for my husband, myself and my son, which was, you know, $715 a month for seven months. On top of it, all the other bills on top of, you know, a lack of income, they just — you go bankrupt.
AMY GOODMAN: In fact, you’re not alone. The studies who, I think in 2007, the majority of people who went bankrupt went bankrupt because of medical expenses, and the vast majority of them, like 80 percent, had insurance.
STACIE RITTER: Yes.
AMY GOODMAN: Juan?
JUAN GONZALEZ: Well, I just want to ask you, as you hear all this debate in Congress about health insurance reform and providing better health insurance for Americans, you’ve decided, actually, to put your body on the line and protest outside of CIGNA. Your concerns, as you hear the people in Congress debate this issue?
STACIE RITTER: Well, my concerns is they’re going to go ahead and be bought out by the big drug companies. You know, the Democrats now are selling out. They are choosing their own greed and self-need over the needs of the American people.
One of the reasons why this is so important to me is my children, who are cancer survivors now, are going to be deemed — you know, they’re marked with a pre-existing condition. And if things continue the way that they are — God forbid, my husband would lose his job; they’ve already taken pay cuts and stuff in order to not have to let people go — but what would happen? Nobody would want to pick me and my children up on an insurance plan. And as soon as my kids grow up and they graduate college, they’re going to have to go out and try to get insurance that way, and nobody is going to cover them, not as things are right now. And I know how slow things work. So we’ve got to change this, and we’ve got to change this now, in order for children who are eleven years old to be able to access the healthcare and the need, you know, to take care of their health needs as adults.
AMY GOODMAN: Stacie Ritter, we want to thank you very much for being with us, and best to Madeline and Hannah, your identical twin daughters.
STACIE RITTER: Thank you.
AMY GOODMAN: This is Democracy Now!, democracynow.org, The War and Peace Report. If you want to see pictures of the family and the daughters, you can go to our website at democracynow.org.










Media Options