
Related
Guests
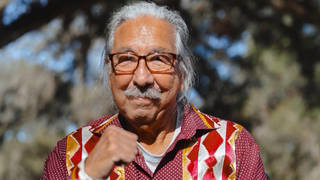
- Abraar Karaninternal medicine doctor and infectious disease fellow at Stanford University School of Medicine.
Governments around the world are eagerly returning back to pre-pandemic conditions by relaxing preventative restrictions, lifting mask mandates and pulling back public funding. Dr. Abraar Karan, infectious disease fellow at Stanford University School of Medicine, says these moves are overly optimistic and that the U.S. is not prepared for new variants spreading around the country. “We’re trying to say it’s over. It’s not true,” he says. “As time goes on, immunity wanes, and we will begin to see more severe cases.”
Transcript
AMY GOODMAN: On Thursday, WHO’s Director-General Tedros Adhanom Ghebreyesus warned the world is playing with fire in its handling of the pandemic.
TEDROS ADHANOM GHEBREYESUS: Coupled with low investment in early diagnosis, it’s simply not acceptable that in the worst pandemic in a century innovative treatments that can save lives are not reaching those that need them. We are playing with a fire that continues to burn us. Meanwhile, manufacturers are posting record profits. WHO supports fair reward for innovation, but we cannot accept prices that make lifesaving treatments available to the rich and out of reach for the poor. This is a moral failing.
AMY GOODMAN: That’s the World Health Organization’s director-general.
We are also joined by Dr. Abraar Karan. He is a fellow at Stanford University, an infectious disease doctor.
If you can comment on what he’s saying? Talk about the world record we are now seeing. Also, you have family in India, where it is believed to be 10 times worse than is being discussed. And you’re here in the United States, that has just passed this horrifically grim milestone of 1 million COVID deaths.
DR. ABRAAR KARAN: Thanks for having me, Amy.
You know, what the director-general is saying is absolutely correct. And as somebody who’s worked in global health for now over a decade, I’ve seen that this was the weakness that we were all worried about, you know, particularly that if we were hit with a pandemic like this, that countries would turn inwards instead of working together, that access to lifesaving medications and vaccines would primarily be focused in high-income countries and that the idea of global health equity, the idea that all lives matter regardless of where you live, that those ideas would take really a backseat to the interests of wealthy countries. And we saw this play out even with the Ebola epidemics, right? So, we saw with Ebola in West Africa, once it started to spread and there was a threat of cases coming to Europe or the United States, that’s when there was a lot more investment and interest and attention. And so, when there was a subsequent outbreak in the DRC, there was a lot more focus on it at that point than there had been, even though the DRC had suffered many Ebola outbreaks.
You know, we have seen in global health, especially around pandemics, that the focus is on global health security: How do rich nations keep cases from coming in? And this is what we saw as the response when Omicron was detected in South Africa and South African scientists very graciously shared their expertise with the world to alert as quickly as possible that there was this new variant that was spreading quickly. And the response was to close down borders. And that was not the right move. That was not something that was going to help. And it was really just a show of the lack of equity and the lack of partnership between wealthy — wealthier countries and lower-income countries. And we’re seeing the same play out now, as the good doctor said before me, you know, in terms of therapeutics access to Paxlovid, access to mRNA technology. We’re continuing to see pharmaceutical companies and other companies driven by profit.
And to bring it back to what the director-general was saying, we are playing with fire, because we are seeing BA.4, BA.5 now in South Africa. We’re going to see even more variants over time. And we don’t know, we can’t predict: Is it going to be more virulent the next time? Is it going to be both more virulent and more transmissible? You know, we’ve already seen monoclonal antibody treatments be no longer effective against newer variants. We’re seeing that, as time goes on, we can’t develop new vaccines fast enough to get us out of a surge. So, if we’re hit with another surge quickly, revaccinating the whole population of countries takes time, and we will be hit so hard once again. In the U.S., we’re only at about 30% boosted. And that, too, if you look by certain areas, certain states, it’s even less. And, you know, a lot of people didn’t get vaccinated since last year. And clinically, I know that as time goes on, immunity wanes. We will start to see more severe cases, even amongst people that were previously vaccinated.
AMY GOODMAN: And, Dr. Karan, this statistic we cited, the 50% increase for transit workers at the airports, increase in COVID-19, the significance of this, of course, a few weeks after a Trump appointee judge struck down the mask mandates?
DR. ABRAAR KARAN: I mean, this is, one, not surprising. You’re having people who are packed together in indoor settings. This is where the virus transmits most effectively, through primarily short-range aerosol spread but also longer-range aerosol spread. And people are basically getting infected and then going off to work at their workplaces, or they’re traveling, going to different states or different parts of states. And essentially, this is how outbreaks will continue to seed.
So, you know, for me, I was extremely disappointed to see the mask mandate removed in our highest-risk setting, where people are — not only are they packed together and going to different places, they have to go on public transit. I mean, some of our poorest workers, who don’t have private transportation, literally rely on public transportation to get to their jobs. These are where we’ve seen in poorer households, in more crowded households, that the spread has been significantly faster. There is data from Los Angeles showing the secondary attack rate many folds higher in poor Latino households. And so, you know, the implications of this are huge.
When I took — I’ve been taking care of COVID patients since the very start of the epidemic. When I saw, initially, the cases that were coming into the emergency room, they essentially were entire families. It would be one family member who was working, then everyone else got infected, including elderly parents. And we don’t have a good way to slow down home-based spread. I mean, I’m now trying to start up a study here through Stanford to look at interventions we can give to people to filter the air better in their homes when someone gets infected. But we still have a lot of data we need to generate on this.
AMY GOODMAN: Talk more about that.
DR. ABRAAR KARAN: So, essentially, what I’m trying to do is, when somebody gets infected, when an index case comes in — they’re coughing, they get infected with COVID — we want to send them home with an air filtration device. I’m working with air experts here at Stanford who are also going to be part of the team, and working with community health workers, to essentially send them home with an air filtration device, N95 masks for the entire family, instructions on how to safely create better ventilation within crowded spaces, and then call them every day for five days through a community health worker and essentially try to do our best to slow down spread to other family members.
And, you know, we want to get this infrastructure started, because we know that there are going to be big surges again. We know that people are going to be requiring new vaccinations again. And we want to just, essentially, give the resources to families that don’t have them, and really test this in the real world to see if this can slow down home-based spread of the virus. And so, you know, I’ve applied for a grant for this already, hoping the money comes through, that we can get this project started this year.
AMY GOODMAN: Can you talk about the fact that the COVID bill was stripped from the appropriations bill in mid-March, asking for $22.5 billion? The partial funding agreement is back on the table, but it eliminates the $5 billion Biden requested for global vaccination efforts. And even if someone doesn’t care about the rest of the world but is deeply concerned about national security at home, I mean, if the pandemic has taught us nothing, is that if one person is sick somewhere, we are all vulnerable.
DR. ABRAAR KARAN: I couldn’t have said better myself. I mean, we are as vulnerable as the most vulnerable people in our society. And, you know, we saw this. I mean, this played out in real life. Frontline workers got sick first. Everyone else that was wealthier and could stay home stayed home, but eventually they got sick, as well.
And again, if we do not commit to global vaccine equity in a very serious way — this is beyond money, right? This is more than just the money. This is also getting the technology over there, the supply chain issues, the actual rollout. I mean, we saw how hard the vaccine rollout is here. We only have 30% boosted. So there is a lot of work that needs to be done on this front.
And, you know, pulling back on funding is essentially saying that we think the pandemic is over. It’s not over just because we want the pandemic to be over. It’s not over. I mean, the White House Correspondents’ Dinner, the Gridiron Dinner, these are events where we’re trying to say that it’s over, you know, that there’s nothing to worry about. And this is not true. I mean, this is frankly not true.
When you have epidemic-level spread, society shuts down. People cannot work when they’re sick. When I got Omicron in January — yes, I’m young, I’m healthy, I was boosted — I had to be out of work for 10 days, and I’m an infectious disease doctor. You know, if you have people out of work, you functionally cannot continue. And Omicron showed us that, right? People said after Delta the same thing: “You know, a lot of people have been infected. People have been vaccinated. We’re not going to have to worry.” And then Omicron hit, and pretty much anyone that was unvaccinated was pretty high risk of getting it. And we saw people get very sick from Omicron. I took care of these patients in the hospital.
So, you know, you hit the nail on the head, that pulling back on funding to say, “The pandemic is over. Let’s focus on other things. Let’s just get over it,” that’s not a strategy, and it’s just not true.
AMY GOODMAN: But, finally, the — we have 15 seconds. The new subvariants spreading through the United States?
DR. ABRAAR KARAN: Yeah. So, there’s the BA.2.1.2.1. And this variant was, you know, first spreading in New York. At the end of last week, it was about 36% of new cases. In a few weeks, it’s going to be potentially most of new cases, if not all of them. You know, right now we don’t have data to suggest that it’s more severe, but it probably is more transmissible, and it’s outcompeting the old strains of Omicron. So, this is going to continue to happen, right? Until we get better ventilation in shared indoor spaces, global vaccine equity, better rollout of Paxlovid, better rollout of boosting, newer vaccines, we are going to be in trouble, and if not now, soon.
AMY GOODMAN: Dr. Abraar Karan, I want to thank you for being with us, infectious disease doc at Stanford University. Thank you for joining us. We’ll also link to your writings at democracynow.org. Achal Prabhala, thanks so much also, coordinator of the AccessIBSA project, which campaigns for access to medicines in India, Brazil and South Africa.
When we come back, we speak with law professor Michele Goodwin, author of Policing the Womb: Invisible Women and the Criminalization of Motherhood. Stay with us.
[break]
AMY GOODMAN: “Light of a Clear Blue Morning” by Dolly Parton. On Wednesday, it was announced that she will be receiving a Rock and Roll Hall of Fame honor in the 2022 class.









Media Options