
Topics
Guests
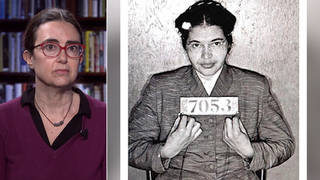
- Dr. Diane MeierDirector of the Center to Advance Palliative Care and the Lilian and Benjamin Hertzberg Palliative Care Institute at Mount Sinai School of Medicine here in New York. She has received numerous awards, including a MacArthur Genius Grant, and is currently working with the Senate Committee on Health, Education, Labor & Pensions.
As President Obama signs the landmark heathcare bill into law, we look at palliative care — the care needed by people struggling with serious illnesses. We’ll talk to a pioneer in the field, Dr. Diane Meier. [includes rush transcript]
Transcript
AMY GOODMAN: On Tuesday, President Obama signed the landmark healthcare reform bill into law. The move came after more than a year of debate in Congress and around the country about healthcare reform. Some of the strongest rhetoric in the debate came during the summer, when Republicans began attacking components of the bill, saying they amounted to “death panels.” They were referring to provisions that would have required doctors to discuss end-of-life questions with terminally ill patients. Those provisions were taken out and were not part of the bill Obama signed yesterday.
Well, today we turn to take a serious look at the aspect of medical care that often goes unnoticed. I’m talking about palliative care needed by people struggling with serious and sometimes terminal illnesses.
I’m joined now by a pioneer in the field. Her name is Dr. Diane Meier. She’s director of the Center to Advance Palliative Care and the Lilian and Benjamin Hertzberg Palliative Care Institute at Mount Sinai School of Medicine here in New York. She has received numerous awards, including a MacArthur Genius Grant. She’s clearly working with the Senate Committee on Health, Education, Labor and Pensions, known as HELP. Dr. Diane Meier joins us now from Washington, DC.
Welcome to Democracy Now!, Dr. Meier.
DR. DIANE MEIER: Thank you, Amy. It’s wonderful to be here.
AMY GOODMAN: It’s great to have you with us. And just in the interest of disclosure, I met Dr. Meier at Mount Sinai when my mother was struggling in the last weeks of her life. She died on October 5th. Today would have been her eightieth birthday. And meeting Diane Meier exposed my family to this remarkable field that we had known very little about. To start, Dr. Meier, tell us what palliative care is.
DR. DIANE MEIER: Palliative care is a medical and healthcare specialty that focuses on starting with the patient and their family and making every effort to reduce or eliminate suffering, whether it’s from pain or depression or fatigue or worry, and helping patients and families get what they want from the healthcare system.
AMY GOODMAN: You deal with people at the end of their lives, but not always. Explain how that works.
DR. DIANE MEIER: Well, there’s a common misconception that palliative is the same as hospice. Hospice is a version of palliative care that is specifically for people at the very end of their life who are no longer going to benefit from curative or life-prolonging treatment. Palliative care, in contrast, is appropriate from the point of diagnosis of a serious illness, whether you’re going to live with that illness for ten years or ten days.
The goal of palliative care is to help people live as well as possible for as long as possible while they are coexisting with one or more chronic conditions. And in your mother’s case, that was a recent and sudden diagnosis of cancer. In many of our patients’ cases, it’s things like heart failure or emphysema or dementia that people live with for years and years, but the burden of the illness is quite significant. And what our team tries to do is to lighten that burden and make those additional years worth having.
AMY GOODMAN: Dr. Meier, talk about the role of pain — yes, in sickness, but also in wellness and in how people can cope — and how it’s treated by the medical profession today.
DR. DIANE MEIER: Well, we now know that pain is extremely debilitating and is a major risk factor and predictor for depression, for other illnesses, for social isolation, and actually for increased risk of death. So this notion that somehow pain is purifying or that it’s noble to suffer with the pain or that it has a certain moral positive valance to grit your teeth and suffer through it is actually completely false. And we now know that untreated pain is really bad for your health, aside from the fact that it causes a great deal of suffering.
Unfortunately, most physicians and nurses receive little or no training on the identification and appropriate treatment and safe treatment of pain. And as is true in many professions, when there’s an area that you don’t know much about and you’re not very comfortable with, most people tend to assume it couldn’t be that important, because if it was really important, then they would have been taught how to deal with it and how to take care of patients with it. So we do see a lot of the health professions turning away from patients who are in pain or minimizing the importance of treating that pain, mostly because those health professionals actually don’t know how to address it. And one of the things that the palliative care field is heavily focused on doing is improving the training of the next generation of doctors and nurses and other health professionals, so that people in pain will have the expertise — have access to the expertise they need, because there are a number of ways to safely and effectively treat pain. It’s just that our healthcare providers need to know how to do it.
AMY GOODMAN: For people who want to chime in here or ask a question or weigh in, you can email at stories(at)democracynow.org. That’s stories(at)democracynow.org. We’re speaking to Dr. Diane Meier, director of the Center to Advance Palliative Care Institute at Mount Sinai School of Medicine here in New York.
How do you deal with the pain? What exactly do you do? And what do you do differently than, well, conventional medicine?
DR. DIANE MEIER: Well, I think the most important thing that we do is recognize how important it is and recognize that if a person is in pain, nothing else can really be accomplished. That is, they can’t interact effectively with their families. They can’t accomplish important goals to them. Very often they can’t even get out of bed in the morning, because the pain is draining all their strength and energy. So we begin by understanding that pain is basically a medical emergency, and it’s very, very important to address it and work with the patient to get it under control.
The second step is to ask the patient about the pain and to believe the patient about their pain. Believe it or not, many health professionals have been kind of trained to be suspicious of patients who describe pain and to worry that perhaps those patients are seeking substances they shouldn’t have or are really hidden addicts looking for access to opiate analgesics and that the pain isn’t real, rather than initially responding by trusting the patient and believing the patient’s report of pain. So that’s the second thing we do.
We not only ask the patient about the pain, we ask them about its severity, and we ask people to rate their pain on a scale of zero to ten, with zero being no pain and ten being the worst imaginable pain. And we’re then able to track the effectiveness of the things we do to try to treat the pain, by asking the patient, “What number is your pain at now?” and explaining to the patient where we want that number to be. So, for example, if a patient tells me that their pain is at an eight or a nine, we’ll say, “That’s completely unacceptable. We want to get that pain level at a four or below. So that’s what we‘re going to work with you on, is adjusting the medication, getting the doses right, managing the side effects, until we can get it to a four or below.” And then we ask the patient, “Does that sound OK to you?” That is, it’s up to the patient where they would — what they want the target to be.
And then we begin by administering medications, usually starting with very low doses and going up very gradually, because each patient is so different in the amount of medicine and the type of medicine they require to get their pain under control. And if someone is in severe pain, we sit at the bedside with the medication and don’t leave until we have gotten that pain under control. One of the things that causes patients the most distress is the sense that even though they report pain, people aren’t taking it seriously, people don’t answer the call bell, doctors don’t respond. So just by sitting there and saying, “We are taking this really seriously, and we’re not going to leave your bedside until this symptom becomes bearable,” that, in and of itself, so dramatically reduces the anxiety and the fear that it goes a long way towards making patients feel like they are in control and they can get the help they need.
AMY GOODMAN: I mean, that was the — what sort of shattered the paradigm for us, is that our mother had to be in so much pain before we could get help, and you coming in and saying, “We have to shift this around. She shouldn’t be experiencing pain, from the beginning.”
DR. DIANE MEIER: Mm-hmm, right. And as you know very well, that, you know, she didn’t get a lot of time after diagnosis, and that time was infinitely precious. And to have it chewed up by trying to suffer through and bear excruciating pain was, you know, stealing something from all of you, and there was no excuse for that.
AMY GOODMAN: Dr. Meier, what about the healthcare legislation and this whole issue of what was taken out of the legislation, and what you think needs to be done, and, of course, the controversy around, quote, “death panels” and what it did to your field?
DR. DIANE MEIER: Well, that notion of death panels was pure lies. There was nothing even vaguely related to the attacks that were on the legislation. All the legislation said was that doctors should be reimbursed by Medicare for having conversations with patients with serious and chronic illness about their goals for medical care. It did not mandate those conversations. It did not require anyone to participate in them. It merely recognized that these are long conversations. They require a lot of time between physicians and nurse practitioners and their patients and families, and that, as it stands now, physicians are essentially not compensated for that.
The result of not being paid for doing those things is that those conversations almost never take place, because physicians are struggling to, particularly those in primary care, make enough of a living to pay their staff, pay their office rent, and be able to pay their own mortgage. So, when faced with those kinds of financial pressures, understandably many physicians are doing — seeing as many people as they can in a day and don’t see that they have time for a forty-five-minute or hour-long conversation with a patient who has a new diagnosis of kidney failure, for example, or a new diagnosis of cancer, to talk with them about the pros and cons of the treatment options, to understand what that patients goals are, what their worries are, what their fears are, to help them understand their choices, and to make good choices for themselves.
All this bill did was say we will compensate physicians for having those discussions if the patients want to have them. And it was twisted and deformed and surrounded by lies, precisely in an attempt to defeat any kind of health reform and also to harm President Obama’s chances of reelection and the election outcomes in the 2010 November midterms. And it was very effective. It was extremely effective strategy. Unfortunately, it bore no relationship to the truth, and it scared the American public, which was the intention, away from getting the information — and information is power in healthcare, as in every other aspect of life — getting the information they need to negotiate the healthcare system in the context of a serious illness.
AMY GOODMAN: So, has it set your field back at this point? And where does it stand with the legislation today?
DR. DIANE MEIER: Well, I had thought that it really set our field back, but when you think back on, for example, the Terri Schiavo debacle several years ago, there was enormous fear in our field that the American public believe that palliative care was about helping people shorten their lives or shortening people’s lives to save money, but actually, the pendulum swung back the other way. The American public is not that easily duped. The American public understands how difficult it is to help a family member through a serious and chronic disease. The American public wants more time talking with their physicians. In fact, that is the number one complaint of patients and families in the healthcare system, is that they don’t have enough time to talk with their physicians about what’s going on. So, while I was quite concerned and distressed by what went on last summer around the death panels, I think the great middle, the great middle of the public, understands that this was hyperbole and hype and it was political and it wasn’t factual, or at least that’s my hope.
So what needs to happen from a policy standpoint, I think it’s certainly important to compensate physicians for listening to and talking to their patients. And that is not in the current bill, but it’s something that we’ll be working on in the future. But it’s also very important to encourage young physicians and young nurses to choose to specialize in this field, because right now we have a lot more demand for people who know something about palliative care than there are people to fill those positions. So I’m hoping the federal government will do something about the workforce crisis that we’re facing, because with the growth in numbers and needs of older adults in our country with illnesses like the one your mother had, but also many other illnesses like dementia or heart disease or kidney failure, there’s an urgent need for more people with training in palliative care, and we’re going to need the federal government to help us meet that need.
AMY GOODMAN: And for people in hospitals now, for people who want to find someone in palliative care, can they just ask? Does every hospital have a palliative care department?
DR. DIANE MEIER: Well, I can’t say every hospital does, but I will tell you that if you’re in a hospital with more than 300 beds, which is where most people with complex or serious illness find themselves in this country, over 80 percent of hospitals of that size do now have a palliative care program. Unfortunately, many patients and families don’t know that those programs exist. So, like in anything else, you have to be an informed consumer. You have to demand to get your needs met. And it’s very — call the hospital operator. Say, “Is there a palliative care program here? What’s the phone number? What’s their beeper number?” Tell your physician that you want consultation from a palliative care team. Often physicians are hesitant to call palliative care in, because they misunderstand and think that palliative care is only about brink-of-death care. Palliative care is about living as well as you can for as long as you can and helping to lift the burden of living with an illness. And physicians need to be educated, and they will be educated by you, the patient, and the patient’s family. But you have to demand what you need.
AMY GOODMAN: And in these last few seconds, how important is the family when someone is sick?
DR. DIANE MEIER: You know, the family — the family is the key to not only the patient’s continued survival and quality of life, but the family also suffers enormously, suffering with their loved one and also suffering because of what they see happening to their loved one as a consequence of the illness and as a consequence of our very broken and fragmented healthcare system. So the family is very much the focus of the work of the palliative care team, because we believe that you can’t help the patient if you’re not also helping the family.
AMY GOODMAN: Dr. Diane Meier, I want to thank you very much for being with us, director of the Center to Advance Palliative Care at Mount Sinai College of Medicine here in New York. And if you’d like to write to us about your own experiences, we’ll continue this, and in the coming days I will do a tribute, a long-awaited tribute, to my mom. I couldn’t quite do it in October, but now, as we would have been celebrating her eightieth birthday this weekend, I’m going to try to pull together all my strength and tell you a little about who this great woman was. But Dr. Diane Meier, thank you for giving us the time, my brothers and I and my extended family, to have quality time with my mom in those last days.










Media Options