
Topics
Guests
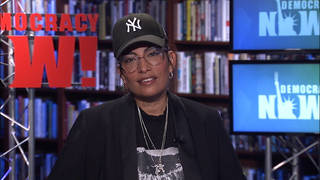
- Monica Peekphysician, associate professor of medicine and health disparities researcher at the University of Chicago.
As distribution of coronavirus vaccines draws near, a recent poll suggests that 42% of Americans are reluctant to take the vaccine. In response, some, including former Maryland congressmember and presidential candidate John Delaney, are pushing to pay people to get vaccinated, a move being discouraged by many, including Dr. Monica Peek, a physician, associate professor of medicine and health disparities researcher at the University of Chicago. She says there are major concerns about how to ensure at-risk groups get vaccinated while overcoming public doubts about the safety and efficacy of the vaccines, but paying people to get vaccinated would be a mistake. “We need to have the public trust that this vaccine will be safe, and we cannot cut corners,” she says.
Transcript
AMY GOODMAN: This is Democracy Now! I’m Amy Goodman, with Juan González, as we continue to look at the coronavirus pandemic spike here in the U.S. and how the vaccine will be distributed, as the CDC prepares to meet today to vote on who should be the first to get the vaccine once it’s available. As distribution draws near, a recent poll suggests 42% of Americans are reluctant to take the vaccine. In response, some, including the former Maryland congressman and former presidential candidate John Delaney, are pushing to pay people to get vaccinated. This is Delaney on CNN responding to criticism that the plan would cause an undue burden on people who are economically disadvantaged.
JOHN DELANEY: Those who are least economically so among us have suffered disproportionately under this pandemic. So many of those people are not sitting at home and Zooming into work; they’re actually getting on public transportation, going to grocery stores and making sure the essential things that we all need are available. They are the people who will benefit the most from getting the vaccination rate up.
AMY GOODMAN: Well, for more on vaccine distribution, we’re joined by Dr. Monica Peek, a physician, associate professor of medicine and health disparities researcher at the University of Chicago. She is meeting at the university today to determine how the university will roll out the vaccine there. In Chicago, like other cities across the country, those killed by COVID-19 have been disproportionately African American and Latinx.
Dr. Peek, welcome to Democracy Now! It’s great to have you with us. Why don’t you start off by responding to what the former congressman is proposing: If there is a problem with people being concerned about the vaccine, pay them to take it?
DR. MONICA PEEK: No. I agree with Dr. Pernell in that we should separate the two issues of economic need and the issue of vaccine implementation, because we don’t want the perception of vaccine safety and trust in the vaccine to cloud the waters of economic need. And so, it is really important that people are able to look at the science, that people are able to follow the words of the scientists and the public health professionals and say, “This is something that is safe that I believe in, that the trusted professionals are recommending that I take,” and that they’re not saying, “This is something that financially I need to do, and I think there might be more risks associated with it because I’m having to be paid to take it, but because I’m so broke, I’m going to put my body in harm’s way in order to get this money.” We don’t want people feeling like they have to make that choice.
So, we need to be able to disentangle those two things and make sure that we have given the people the stimulus that they need. Those conversations are in gridlock. That needs to, you know, fix itself. We need to come to agreement about how to make sure that we are financially supporting the people that are in this economic crisis. Separately, we need to figure out how we’re going to be able to ensure that we have the trust needed to vaccinate our entire U.S. population. Everyone has got to get vaccinated quickly. And so, those are two separate conversations.
JUAN GONZÁLEZ: And on this issue, Dr. Peek, of the getting everyone vaccinated, clearly, there will have to be steps and the decisions that are being made today in terms of priorities at the federal level. How does this — even at your university or at the local level, how do the health professionals — what kind of things do they think about in terms of, after the first responders, the people in the healthcare system, who gets it next?
DR. MONICA PEEK: Well, you know, there are millions of people that need this vaccine. And so, a lot of thought has been going into how to fairly allocate the vaccine, way before we knew that the vaccines would even be ready. So, it’s a miracle that we have two that are coming on the market this quickly. And so, the National Academy of Sciences, Engineering and Medicine had been meeting already for months and has come up with recommendations. The CDC is currently meeting. Individual hospitals are coming up with their individual rollout plans.
But the general consensus is that people who are frontline workers, people who are considered frontline healthcare workers, high-risk healthcare workers, people who are essential workers, those who are sick, have chronic medical problems, those who are living in close quarters, congregate facilities like nursing homes, homeless shelters, prisons, people that are elderly — all of these sort of high-risk populations, for whatever reason, based on your job, where you’re living, how sick you are, those are the populations that need to be vaccinated early — K-12 teachers. We need to be able to get people back into school, into settings where they can be close together.
And so, there’s a phased rollout, where we have, you know, a phase 1, a phase 2, a phase 3, so that we can sort of, in an orderly fashion, figure out who’s going to go first, and ultimately get to make sure that everyone in the population goes. And so, right now we’re trying to think about just phase 1A, which is high-risk health workers and first responders. And so, assuming that things happen on time and, December 10th, the first vaccine is made available and starts being shipped out, then the hospitals are beginning to look inwardly and think about how we’re going to vaccinate our own hospital employee population.
So, where I am, we have about 6,500 employees, a little more than that, and so we think that we can vaccinate everybody in a week. So, if we did a thousand vaccinations a day, then we could get everyone done within a week’s time. And so, we are sort of looking at that kind of time frame.
JUAN GONZÁLEZ: And when we talk about, for instance, first responders and folks in healthcare facilities, I’m assuming that, for instance, in a hospital, that includes not just the nurses and the doctors and the — but also the maintenance staff and the kitchen workers and all the other people that are part of that hospital complex. Is that true?
DR. MONICA PEEK: That is true. Everybody in the hospital is potentially exposed. And we think about when you are a patient in the hospital, someone is coming in to clean your room. Someone is coming in to deliver your food. Someone’s coming in to take your temperature. There are many people that come in and out of that door — deliver magazines — who are not your nurse or your physician but have contact with you. There are people who are changing your bed linens and that are, you know, having contact with soiled, contaminated, infectious products. And so, everybody needs to be protected. We are all in this together. And so, the hospital is a bubble that we’re all in, and we are all at risk. And so, yes, hospital workers means all hospital workers.
AMY GOODMAN: As we were just talking with Dr. Chris Pernell about the use of experimentation especially on the African American community, medical experimentation, one of your specialties is racial disparities. And I had two questions. This isn’t related just to disparities. You said everyone could be vaccinated in a week, but these are a two-part vaccine. So there is this question of: Will they use all the 40 million or so vaccines all at once and then wait for the next ones to be developed, or will they only use 20 million of them, so you can get the second vaccine in whatever that period is? And if you can talk about whether it conveys immunity, or you can actually get sick but you will be asymptomatic and you can still spread it? All these questions about the vaccine. But then also, in the wider population, since that’s what you deal with also outside of the University of Chicago, workers at the meatpacking plants, farmworkers, people who are undocumented, how do we ensure that they all have equal access?
DR. MONICA PEEK: These are excellent questions and difficult questions, but ones that we are going to have to think about, how we have a system in place to roll out implementation. And so, already it shows that this is not something that hospitals, in and of themselves, are going to do. The vaccines are primarily going to be shipped to health departments, and then health departments then parcel them out to different institutions. And so, in some cases, you know, hospitals will be working alongside other kinds of organizations to make sure that populations are effectively vaccinated.
And so, certainly, we are used for caring for patients, and so we will be caring for our own patients who are medically vulnerable, and making sure that they get vaccinated. But some people — not everyone has a primary care physician. Many people exist, unfortunately, without routine care. But we need to make sure that everyone in this country is vaccinated. And so we’re going to have to think about non-healthcare sites for vaccination, just like we’re doing for COVID testing, where we have pop-up testing sites. We’re going to have to be more creative in how we think about reaching populations that don’t ordinarily show up at our doors for care and to ensure that we are reaching everyone for vaccine delivery.
JUAN GONZÁLEZ: And, Dr. Peek, I wanted to ask you — given the fact that the vaccine will be rolled out probably right around the time that the deaths and the hospitalizations from the virus are at record levels, there’s going to be enormous pressure by sectors of the population to get the vaccine. I’m thinking, over the last nine months, there’s a whole section of the American public that has had the ability to work remotely from home and therefore protect themselves, whereas those workers who have to go to work every day have been increasingly the ones most exposed. So, shouldn’t the vaccine then be rolled out to those who are being forced to work every day as a result of the kind of jobs that they have? And won’t there be pressure from those who are generally more professional, more middle-class, who have stayed at home all these nine months, to also get the vaccine? How do you monitor? What’s going to be the monitoring process to make sure there’s not abuses?
DR. MONICA PEEK: Yeah, you know, that’s an excellent question. I am unaware of sort of the teeth or the penalties for people jumping in line and trying to abuse the system. But what we have tried to put in place are parameters and a rollout system, so that — you know, think about a buffet line on a cruise ship or something. So, now we’re taking people who are having the blue cards. These are the people who are due to get vaccinated. You know, this week we’re doing everyone who’s a healthcare employee. Next week we’re doing essential workers, for the next month. And we’re going to figure out exactly how we find those people and whatever. You know, those are the plans and implementation policies and things we’re going to have to be working through in conjunction with city planners. And this is where the rubber hits the road, and all of the infrastructure and planning has to start working and has been working.
But essential workers, that are keeping our cities and townships functioning, they’re high up on the list. They’re part of the phase 2. And so, again, people who are performing critical functions for the city, as well as people who are carrying higher burdens of disease, are priority people. Frequently, those are the same people, because people who have been burdened by oppression, by structural inequities and racism, that has affected their health. And the same structural inequities has meant that they have had limited opportunities as far as education and career advancement, so a lot of times they’re more likely to be working in essential worker jobs. And so, many of the people that we’re talking about being high priorities for a medical reason or for an occupational reason are the same people. And so those people may have multiple reasons to be priority individuals for getting vaccinated.
AMY GOODMAN: And, Dr. Monica Peek, maybe we’re getting ahead of ourselves here. I mean, you have Stephen Hahn, head of the FDA, the doctor who’s been called to the White House because Mark Meadows, the chief of staff, who also came down with COVID, as did President Trump — of course, the White House is a hot spot because of the herd immunity approach President Trump has taken — putting pressure on him to speed up the approval process. It will be going to the FDA, but then it has to be approved by the CDC. This has been done at unbelievable speed, which is both the excellent news but also a concern for people. Is this being approved with the kind of scientific review that something like this, distributed on a mass basis, needs? Are you concerned about that — overall, the speed with which this is being done, and the fact that even before January 20th, as everyone looks at that next Inauguration Day, you have tens of thousands of Americans who will die, and what President Trump needs to be doing right now, outside the virus — outside the vaccine, to ensure that people have access to masks and tests, something that continues to be a massive problem in this country?
DR. MONICA PEEK: Yes, so much you just said right there. So, where to start? I guess the easy answer is thinking about the current administration. Given that Trump has been in office for four years, and we’ve seen what he can and cannot do, and we’ve seen how he has handled and approached the COVID pandemic, I don’t have high hopes that his behavior will change between now and January 20th. The best that I can hope for is that he will step out of the way, in enough way to make room for the incoming Biden administration and the transition team to be able to make some headway.
Biden has — the first thing he did was pull together his COVID-19 task force, which is chocked full of scientists, health policy analysts, public health professionals, people who are very experienced in vaccine policy and know what they’re doing. And so, getting these people together, who have already been thinking about COVID for years — well, not for years, but, you know, infectious disease for years and have been thinking about the COVID pandemic since it started — you know, that is where we need to be able to let these people flourish in this space, have access to some resources.
But I do think that talking about just the rapidity with which these vaccines have moved forward, you’re right in that that’s a good thing, and then there’s some ambivalence there. We want things to move as quickly as possible, as long as it’s safe. We want them to move with the speed of light, as long as the science is there, and for them not to have been politically approved, but for them to have been scientifically approved. And so, that’s the fine line that we want to walk. And so, when all the scientists have come together behind the idea of Project Warp Speed, that has been, so far, an effective scientific endeavor. And so we want that kind of scientific collaboration to continue. But what we don’t want is politicians getting in the mix and saying, “I really need this to happen to ensure my reelection,” or, you know, things that worry the public. And we know that these things have worried the public.
And so, we cannot undermine — or, we have already undermined. We cannot continue to undermine and erode the public trust in this process. We need to have the public trust that this vaccine will be safe. And we cannot cut corners, because once the vaccine is here, if no one is willing to take it, all of this effort will have been for naught. So we can’t, you know, speed things up just to get here, and then no one is willing to use it. So we have to, as Dr. Pernell was saying, do the hard work. We have to do it right. We have to think right now, in advance, about how we’re going to make this vaccine acceptable to communities who are thinking that this is something that I’m not interested in, and be engaging right now in campaigns of truth-telling. We have to be engaging with organizations that we know are trustworthy. Rather than tearing down the CDC, we need to be building up that public health infrastructure, reinvesting in the CDC, giving them back the leadership and the ability to tell truth to the public, and giving them back the right to run the ship.
AMY GOODMAN: Dr. Monica Peek, I want to thank you so much for being with us, physician, associate professor of medicine and health disparities researcher at the University of Chicago. There is so much to talk about, and we will get back to you soon.
Again, next up, it’s World AIDS Day. We’ll speak with professor Steven Thrasher in 30 seconds.
[break]
AMY GOODMAN: António Variações, a gay icon in Paraguay, who died from HIV/AIDS in 1984.











Media Options