
Guests
- Dr. Camara Phyllis Jonesfamily physician, epidemiologist and past president of the American Public Health Association. She teaches at the Rollins School of Public Health at Emory University and at the Morehouse School of Medicine.
As the first shipments of a federally approved COVID-19 vaccine arrive across the United States, healthcare workers and residents of nursing homes will receive the first shipments, and epidemiologist Camara Phyllis Jones says communities of color with high rates of COVID-19 should also get consideration for early access. “I think that CDC got it right partially in terms of those overexposed because of their work or their living conditions, but they did not include our brothers and sisters in prisons, jails, detention centers, and they did not include those of us who are more exposed and less protected in our work,” say Dr. Jones, who is the former president of the American Public Health Association.
Transcript
AMY GOODMAN: This is Democracy Now!, democracynow.org, The Quarantine Report. I’m Amy Goodman.
The first shipments of the federally approved COVID-19 vaccine are arriving today at 145 locations across all 50 states. This comes as the U.S. death toll hits 300,000 — by far the highest in the world. On Friday night, the Food and Drug Administration issued emergency use authorization for the Pfizer-BioNTech COVID-19 vaccine. The first shipment of the vaccine will cover nearly 3 million people. Healthcare workers will receive the first doses, some possibly as early as today. Residents of nursing homes will be next in line. Another coronavirus vaccine, one developed by Moderna, could be approved as soon as the end of the week. As the U.S. government races to distribute the vaccine, there are many questions over who should get the first shots and what steps the government can take to build trust in the vaccine.
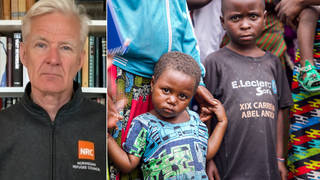
We’re joined now by Dr. Camara Phyllis Jones, the past president of the American Public Health Association, a family physician, epidemiologist, longtime antiracism activist. She’s joining us from Atlanta, Georgia, where she teaches at Emory Rollins School of Public Health and the Morehouse School of Medicine.
It’s great to have you back, Doctor. You’re joining us on the first day of early voting in the Senate runoff races that could determine the balance of the Senate. But we’re here to talk to you about who should get this vaccine. Can you talk about how it’s being rolled out and how that decision is made?
DR. CAMARA PHYLLIS JONES: Yes. Thank you for having me back.
And the Advisory Committee on Immunization Practices, which advises the CDC, met a few weeks ago and proposed that healthcare workers and people who are living in long-term care facilities receive the vaccine first. And I agree that those who are more exposed through their work or through their living situations should get the vaccine first, but I think that the panel actually neglected to recognize that not only are healthcare workers more exposed through their work, but other essential workers are exposed through — you know, those in transportation sectors, those in the food chain and warehouses and the like. And those essential workers even tend to be less protected in their increased exposure, so I think that those essential workers should be included in the first rollout.
And then, also the advisory committee recognized that residents of long-term care facilities are more exposed because of their living situations, and so they talked about nursing homes and assisted living facilities, but they did not talk about those who are in long-term care facilities in prisons, in jails, in detention centers. And I think that those people, as well, should be offered a first chance to get the vaccine.
After those groups — and I would have to say one more group which is at high risk because of their living situations are people who are living in segregated communities — Black and Brown and Indigenous, you know, like Navajo Nation — communities where we’ve seen a very high prevalence of the virus and higher death rates. And so, those people should also be given priority access to the vaccine.
After that, then others of us who have so-called preexisting conditions — so, you know, obesity, cancer diagnoses, kidney disease and the like — as well as those of us who are 65 and over, should be in the next wave.
But I think that CDC got it right partially in terms of those overexposed because of their work or their living conditions, but they did not include our brothers and sisters in prisons, jails, detention centers, and they did not include those of us who are more exposed and less protected in our work.
AMY GOODMAN: So, I want to go to the issue of prisoners, who are in prisons around the country, that have clearly become hot spots for COVID-19. Can you talk about the case for vaccinating prisoners early? You have people like the governor of Colorado, for example, Jared Polis, who said, no, they should not be injected early, given the vaccine early. You argue otherwise.
DR. CAMARA PHYLLIS JONES: I do argue otherwise. I can’t even fathom the devaluation of the lives of prisoners that must be going through the mind of that governor. I mean, if you’re looking at the science and you’re looking at hot spots and you’re looking at conditions where there is going to be a lot of concentrated spread — people are unable to physically distance, they do not have protective equipment — you know, these are the lives that we need to value and save.
Actually, I would say that there are three principles that I’ve articulated for being about health equity, racial equity, social equity. And the first of those is valuing all individuals and populations equally. And when you value somebody, you protect them. You invite their input. You celebrate them. There are lots of things. You invest in them. But certainly, we need to recognize that these are our brothers and sisters. They have been put in danger. We need to decarcerate as much as possible, continue getting them out of danger. And for those who remain incarcerated, we need to offer them the protection that they need.
AMY GOODMAN: And, of course, detention centers, as well, where immigrants are in prisons all over the country and along the border — again, hot spots — and particularly when it comes to the issue of prison authorities moving prisoners from one prison to another, causing superspreading events. In California, for example, coronavirus cases inside prisons have once again skyrocketed, with more than 4,000 active infections among prisoners, the highest number since the pandemic began. Altogether, after 22,000 prisoners tested positive for COVID-19 in California and at least 90 have died, prisoners at San Quentin said authorities are preparing to transfer people to other prisons, despite the COVID-19 levels being at an all-time high. This is award-winning incarcerated journalist Juan Haines, who spoke to Democracy Now! from San Quentin.
JUAN MORENO HAINES: The problem with the transfer is all California prisons are enclosed and unventilated. All throughout the state, our leaders are telling us to stay at home, don’t mingle with people that you don’t know, wear a mask inside — and which we’re all doing that inside of these buildings. But I know we can’t be operating on alternative facts when it comes to enclosed, unventilated buildings. We can’t have one set of rules for restaurants, gyms, nail salons, etc., and another for prisons.
AMY GOODMAN: Award-winning journalist Juan Haines, speaking from inside San Quentin. He reportedly is being transferred as early as today. The responsibility of authorities when it comes to the people that they incarcerate, what they should — their responsibility in caring for them?
DR. CAMARA PHYLLIS JONES: I’m sorry? I didn’t quite —
AMY GOODMAN: If you can discuss the responsibility of federal authorities or state authorities —
DR. CAMARA PHYLLIS JONES: Yes
AMY GOODMAN: — when it comes to who they incarcerate, and caring for them when they’re inside?
DR. CAMARA PHYLLIS JONES: Well, I mean, they do have a responsibility. They have a responsibility of care and a responsibility of protection. But even if they didn’t care about those people, the people that they have so often dehumanized, the people who have been overpoliced in their communities and oversentenced and the like, we have to also recognize that what happens inside the prisons gets into the community in a number of ways. There’s so much churn in terms of Black folks and Brown folks being in and out of prisons. They’re people who work in the prisons.
So, of course we need to value all of us equally, but even if people did not, the self-interest in terms of superspreader events not being constricted or maintained inside the prisons but getting into the communities should also motivate. But clearly, we need to — these people are people. These are our brothers and sisters. As Bryan Stevenson says, we should not be judged by the worst thing that we’ve done in life. We are so much bigger than the worst thing we’ve done in life.
AMY GOODMAN: Even bars do not prevent the transmission, obviously, of coronavirus, and this applies to guards, as well. Dr. Camara Phyllis Jones, you have called for a secretary of equity. Explain.
DR. CAMARA PHYLLIS JONES: Yes. Well, I believe that the Biden-Harris administration already recognizes the importance of infusing attention to equity throughout all of the administration and all of our efforts. When I talk about a secretary of equity, it would be a role that would acknowledge these three principles for achieving health equity: valuing all individuals and populations equally, recognizing and rectifying historical injustices, and then providing resources according to need — not equally, but according to need — which requires developing a metric of need and then having the political spine to distribute resources based on that.
This secretary of equity would interdigitate with all of the other departments, so helping the Transportation Department figure out how do we value all individuals and populations equally, how do we recognize and rectify historical injustices, how do we provide resources according to need — immigration, education, housing, labor, justice, all of these departments with the same guiding principles — and then making those — operationalizing those principles within their wheelhouse, within their realms? And I think that this is very important. We need — in order to get to racial justice, economic justice, climate justice, as well as health justice, we need to be about equity in all of our work. It can’t be something — so, I would just say one more thing about this. With a secretary of equity, it shouldn’t be that equity is all there, and all the other departments are free to go, right? This would be something that would be, I would say, perhaps across the departments. And the Biden-Sanders unity task force has been making similar calls. So, I’m hopeful that something like that will be established.
AMY GOODMAN: At an event hosted by the National Urban League Tuesday, Dr. Anthony Fauci credited African American scientist Dr. Kizzmekia Corbett for helping to lead the development of one of the key vaccines. This is Dr. Corbett, a senior research fellow working with the Vaccine Research Center, speaking in a report by ABC News.
KIZZMEKIA CORBETT: What I want people to understand is that the safety and the development of these vaccines is not any different than what has been happening before. The requirements from the FDA are actually more robust than they have been before. I also understand that there are issues of lack of trustworthiness. And I say it in that way because, understanding that the onus of gaining the public’s trust lies in the hands of people like me from the vaccine development standpoint and the institutions where I am employed, for example, to earn trust that has been stripped from people over the course of centuries, I wanted to make it clear that the work that we’ve been doing for so long, I personally — I stand by it, with essentially all of my being.
AMY GOODMAN: That’s Dr. Kizzmekia Corbett of the National Institutes of Health, who helped to develop the vaccines. Dr. Camara Phyllis Jones, can you talk about her significance?
DR. CAMARA PHYLLIS JONES: Oh, well, it’s amazing. She’s an amazing scientist. I had the opportunity to be on a panel with her sponsored by the Congressional Black Caucus Foundation. If people are interested in that panel, they can look at that September 16th event.
It is important that she’s been leading the science. I would say that I agree that our evaluation has been done by scientists and not by the politicians. I will say that the first vaccine that has received emergency use authorization has shown amazing ability to stop symptomatic disease. We have early safety data, which reassures us, but there remain many questions. And so, part of being trustworthy is not trying to convince or coax or cajole anybody into taking a vaccine; it is to hear people’s questions and then answer their questions truthfully and clearly, where some of the answers right now may be “We don’t know.”
So, we actually don’t know, because the typical amount of time that somebody has been followed after their second dose is two months. So we don’t know about six-month or one-year complications. They followed 40,000 people, so we don’t know about rare complications that might occur in one in 100,000. But all said and done, I know that I would rather live with the uncertainty of having taken the vaccine as opposed to the premature death associated with COVID-19. So when my turn comes in line to get the vaccine, I’m going to accept it. But we have to continue strong safety monitoring as we roll out the vaccine, so that we can answer some of the questions that remain unanswered so far.
AMY GOODMAN: So, talk about why people, particularly African Americans and Latinx and Native American people, are concerned about this vaccine, looking at the history of experimentation. I wanted to turn to Dr. Leon McDougle, the president of the National Medical Association, the NMA, which represents African American physicians and their patients. The NMA launched a COVID-19 task force this summer in hopes of providing one central place for reliable coronavirus information for the Black community. He spoke to the PBS NewsHour.
DR. LEON McDOUGLE: We wanted to be that trusted source and have a independent, nonpartisan lens looking at the data to form a bridge of clarity to help people to understand what in fact is true and what in fact is fiction. … This is part of what I do every day. Doctor means to teach. It is not a dictatorship. We negotiate. We discuss patients’ concern about a particular possible side effect. It’s informed discussion, informed consent. That’s what we do as healthcare professionals.
AMY GOODMAN: That’s Dr. Leon McDougle, president of the National Medical Association. Here in New York today, the vaccine coordination center goes into effect as a massive public education campaign goes out in New York City, for example, as it’s happening all over the country. But this distrust — he was just talking about informed consent, something certainly African Americans did not have when it came, for example, to the Tuskegee experiments, that led to the deaths of so many African American men thinking they were being treated for syphilis when they were left to die.
DR. CAMARA PHYLLIS JONES: That’s right. And the distrust is not just based on historical. There have been many historical abuses, from the use of slave women without anesthesia to perfect gynecological procedures by Marion Sims, who is lifted up as the father of gynecology, by, you know, what they call a Mississippi appendectomy, the sterilization, the forced, without consent, sterilization, including also in Puerto Rico and many places. There have been so many — such a long history of abuse of Black and Brown and Indigenous bodies in our society by the medical profession. But these are not just in the distant past; they continue today. I mean, just months ago, we were hearing about, in one of the detention centers, people who were getting hysterectomies without their knowledge.
So, this trustworthiness is a very important thing that is not on the part of people to trust, but others to evidence their trustworthiness, which has to go beyond the vaccine. It has to be in supporting people through this pandemic by providing a living wage or, you know, a universal basic income for those of us who have lost their jobs. We have to have eviction moratoria and foreclosure moratoria. We have to provide protective equipment to all of our essential workers, in all of our workplaces. We have to have the Occupational Safety and Health Administration promulgate workplace safety standards in the context of COVID-19 and then regulate people and ensure that those standards are met. We shouldn’t be protecting employers from suits in case people in their employ get sick or die. So, this just trustworthiness not just an isolated, single-lane trustworthiness in terms of the vaccine. If we are going to demonstrate that we value all of our lives, then we have to value all aspects of our lives and not just try to say, “Take the vaccine now. You have to do this for the good of the whole,” when the good of the whole has not been trying to protect each of us.
AMY GOODMAN: Well —
DR. CAMARA PHYLLIS JONES: So, yeah.
AMY GOODMAN: Dr. Camara Phyllis Jones, we thank you so much for joining us, family physician, epidemiologist, past president of the American Public Health Association, teaches at the Emory School of Public Health and the Morehouse School of Medicine, speaking to us from Atlanta, Georgia.
When we come back, the Army has fired or suspended 14 officers, including a general and soldiers, stationed at Fort Hood, where 20-year-old soldier Vanessa Guillén was sexually harassed before she was bludgeoned to death earlier this year. Her family says they’re still pushing for justice, and there’s a bill in Congress. Stay with us.












Media Options