
Health experts are raising concerns that wealthy countries have reserved enough coronavirus vaccine doses to immunize their populations multiple times over, while poorer countries may only have enough to vaccinate about 20%. Reuters reports the World Health Organization’s global plan for delivering COVID-19 vaccines to 91 poor and middle-income countries faces a “very high” risk of failure and could leave billions of people with no access to vaccines until 2024. “What we see is that something like 90% of all the vaccine doses that have been purchased have actually been done directly by countries, mostly middle-income and high-income countries,” says Dr. Krishna Udayakumar, founding director of the Duke Global Health Innovation Center, who has been tracking COVID-19 vaccine purchases around the world. “What we are seeing is a lot of side deals, in essence, where people are trying to also ensure that they are hedging their bets to make this work.”
Transcript
AMY GOODMAN: As coronavirus infections and deaths continue to shatter world records in the United States, vaccines are rolling out across the country with healthcare providers first in line, like respiratory therapist Chestina Schubert at UW Health in Madison, Wisconsin.
CHESTINA SCHUBERT: It’s important, because so many people have died from this. And I wanted to have an impact on my community about this and show them that I’m playing my part and getting vaccinated. And I think that I want to inspire people, especially the patients that look like me and I take care of every day, that it’s OK to get vaccinated, it’s safe. And I wanted to put a name and a face, especially here in Madison, Wisconsin, that get vaccinated.
AMY GOODMAN: Meanwhile, in the U.K., 84-year-old retired secretary Maureen Hughes received one of the country’s first Pfizer-BioNTech COVID-19 vaccines and said she now hopes to be able to see family members at Christmas.
MAUREEN HUGHES: I can’t thank people enough that have made this vaccine possible. And when you’ve been isolating for four or five months, you know, this is the product at the end, you know, or beginning — could be the beginning. And we’re just really excited.
AMY GOODMAN: This comes as health experts are raising concerns that wealthy countries have reserved enough vaccine doses to immunize their populations multiple times over, while poorer countries may only have enough to vaccinate just about 20% of their populations.
On Wednesday, Reuters reported the World Health Organization’s global plan for delivering COVID-19 vaccines to 91 poor and middle-income countries — mostly in Africa, Asia and Latin America — faces a, quote, “very high” risk of failure and could leave billions of people with no access to vaccines until as late as 2024.
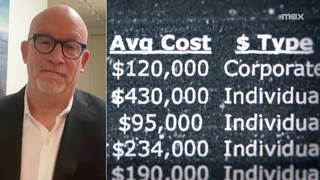
For more, we begin today’s show with Dr. Krishna Udayakumar, founding director of the Duke Global Health Innovation Center and principal researcher for their project that’s tracking COVID-19 vaccine purchases around the world. He’s also a practicing physician at Duke University. Their latest “report”: shows the total worldwide confirmed purchases of COVID-19 vaccines have reached at least 7.25 billion doses, with 3.9 billion of those doses — more than half — in high-income countries, although these countries comprise just 14% of the world’s population.
Dr. Udayakumar, welcome to Democracy Now! It’s great to have you with us. Why don’t you start off by explaining this disparity? And what does it mean that countries hoard vaccines, that they haven’t even gotten yet, to the tune of three times, four times, six times their actual population?
DR. KRISHNA UDAYAKUMAR: Sure. Good to be with you today, and thank you for taking on this important topic.
What we started to see was a tension, where countries are trying to do what’s best for their own populations and at the same time trying to be good citizens of the world. And very quickly, as we saw the pandemic worsen in the spring, we had the development of the COVAX platform, which really brought together the World Health Organization; Gavi, the Vaccine Alliance; and CEPI, the Coalition for Epidemic Preparedness Innovation, each with areas of expertise, aimed at — together, they created a mechanism where the world could come together, figure out how to buy and equitably distribute vaccines around the world. There are now almost 190 countries and participants that have signed on to that model. And yet, what we see is that something like 90% of all the vaccine doses that have been purchased have actually been done directly by countries, mostly middle-income and high-income countries, as opposed to low-income countries.
And so, while, on the one hand, we want to come together into this multilateral platform, what we are seeing is a lot of side deals, in essence, where people are trying to also ensure that they are hedging their bets to make this work. What that means in high-income countries is — I don’t think anybody is interested in trying to hoard vaccines beyond what they need, but much of these purchases were made before we had any idea which of these vaccines might work. So, countries like the U.S., Canada, regions like the EU went out and made a portfolio of bets to buy advance purchases of multiple types of vaccines, not knowing if one or more would actually make it through the very rigorous science to be available.
NERMEEN SHAIKH: And, Dr. Udayakumar, could you talk about what has been said by these rich countries about what they’ll do with all these excess vaccines, vaccine doses? And what countries in the world are being left behind? In other words, what countries are entirely relying on the COVAX facility to get any vaccine?
DR. KRISHNA UDAYAKUMAR: Yeah. We are starting to see positive language from many high-income countries in public statements. Both Canada and the EU, for example, have come out and made clear that if and when they have excess doses available, they envision making those available for low-income countries. What is less clear is whether those are actually going to go through the COVAX mechanism. Or, in the case of Europe, it seems like they may bypass COVAX and make those donations directly to low-income countries.
Now, if the current trend line plays out, what we’re going to see is that most populations in low-income countries are going to be left behind and wait a number of years — two, three, four years — before those populations are really vaccinated at any significant level to achieve herd immunity.
NERMEEN SHAIKH: Dr. Udayakumar, the other vaccines that have not yet been approved from outside the Euro-American world include vaccines, four vaccines, from China that are in late-stage clinical trials, one of which has been approved and is in use in the UAE and Bahrain, as well as the Russia vaccine. Have you been tracking countries that have pre-purchased these vaccines?
DR. KRISHNA UDAYAKUMAR: We have, to the extent they’re publicly available in terms of the information. We do know that there are several countries that have made purchases of various Chinese vaccines. There are several under development. We do know that they have already been used extensively in China. There are public reports that more than a million people in China have been vaccinated with one of the domestically manufactured vaccines, but we don’t have clarity as to which ones they may be. What we also don’t have clarity on are the real data and evidence behind the particular vaccines from China and from Russia.
What we’ve seen from the Pfizer-BioNTech vaccine, for example, and today at the FDA advisory committee we’ll see from the Moderna vaccine, is a very transparent and rigorous process to review and look at all of the primary data to ensure safety and efficacy. Our hope is that we will set very high regulatory standards for all vaccines that come through, and that’s what we envision happening over the coming weeks and months.
And in addition to the vaccines being developed in China and Russia, we know that there are others in the late stage of pipeline development that are also very promising. One developed by Oxford University and AstraZeneca, for example, is in late-stage testing and, when it becomes available, can be scaled up pretty rapidly. And so, we’re hopeful that that’s the type of vaccine that doesn’t require ultra-cold-chain transportation, for example, and storage, that will make it much easier to actually distribute and vaccinate in low-resource settings.
AMY GOODMAN: Doctor, could you explain the whole philosophy behind the COVAX facility, what that means, and also talk about the People’s Vaccine Alliance, that is challenging trade secrets and patents in this time of pandemic, in this time where so many people are dying around the world?
DR. KRISHNA UDAYAKUMAR: Sure. I think both great questions. First, I think COVAX really serves a purpose in developing a truly multilateral approach, which is what we need. We have to recognize that this pandemic is global. The coronavirus doesn’t recognize borders. And we can’t really function as an economy with closed borders for an extended period of time. So, there is a very strong health and economic argument, in addition to the ethical and humanitarian argument, that high-income countries are better off if we can equitably distribute vaccines around the world. For that purpose, COVAX really brings together complementary capabilities, strong global participation.
And yet it has challenges, as you noted earlier in the show, that it’s at very high risk of failing, from their own internal reports. It needs to be financed much more aggressively. It needs a very strong ability to purchase and distribute vaccines in the market. In the midst of not having that in the short term, what we are seeing are mechanisms around, including through some development banks. So, the World Bank, outside of COVAX, has already pledged $12 billion. What we’ve seen just in the last few days is that the Asian Development Bank has put another $9 billion on the table, and the Inter-American Development Bank has put a billion dollars.
So, it’s great to see those funds becoming available, largely directly to countries, so that they can not only purchase — but we have to recognize, just getting the vaccines is the first step. You have to have the distribution and supply chain. You have to have the health workforce. You have to have all of the supplies that go with vaccines to make them available for vaccinations. And you’ve got to have the data and information technology systems to track all this. So, actually getting from vaccine in a vial to a jab in an arm is a hugely complex and expensive task, especially in low-resource settings. So that’s what we also need funding for.
Now, to the second question about intellectual property, it is a major issue, and we’ve seen that be a major issue in prior health — in epidemics like HIV. I’ll preface my comments by saying I am not an expert in IP and have many colleagues who are much more expert at this, but what we’ve seen is a strong recognition of the need for appropriate, equitable global distribution.
On the positive side, some of the indications we’re seeing, is really a ramping up of manufacturing capacity in low- and middle-income countries. Part of the reason India is at a place where they have more than a billion doses potentially coming to their domestic market is because they have the Serum Institute of India, that is a very strong domestic producer but also has become the engine for vaccine manufacturing for the world. They have licensing agreements with the Oxford-AstraZeneca vaccine, for example. We’ve seen manufacturing become available and ramped up in places like Brazil, in Thailand, in South Africa. We think that’s really important to make sure that when vaccine is manufactured in LMIC contexts, low- and middle-income countries, it becomes much more likely that local and regional populations will get access to those. So that’s one trend, without dealing particularly with the IP challenge perhaps, but a mechanism, through licensing or manufacturing capacity, that we are starting to see an uptick in availability over time.
NERMEEN SHAIKH: And, Dr. Udayakumar, right before we conclude, I wanted to ask you about — you mentioned the AstraZeneca-Oxford vaccine, which is more suitable for developing countries because it’s easier to transport, and also that the Serum Institute will be manufacturing it. Do you expect the AstraZeneca-Oxford vaccine to be more readily available in developing countries also because they’ve committed a certain percentage of their vaccines to developing countries, which I don’t believe either Moderna and Pfizer have, though perhaps at this point they have?
DR. KRISHNA UDAYAKUMAR: Yeah, you’re exactly right. So, both India, because of the production at the Serum Institute of India, and COVAX, because of a purchase agreement, will have access to the Oxford-AstraZeneca vaccine. And because it’s a different technology that it’s based on, relative to the Pfizer and Moderna vaccines, it also is able to be scaled much more effectively. The estimates we have is that the manufacturing capacity by the end of 2021 may be as high as 3 billion doses of that particular vaccine. We are seeing that 2.6 billion doses have already been purchased around the world, including by COVAX, including directly by some middle-income countries like India.
So we do see, overall, the fantastic news that we are going to have multiple vaccines available, which would have been unthinkable a year ago or even six months ago. So, we should celebrate the feat of science that’s gotten us this far, but not lose sight that we have to also think about access and equity to make sure that the science is really paying off for human health.
AMY GOODMAN: And also, who does the science. You [sic] tweeted, “You know the two awesome vaccines that will tame the pandemic? Pfizer’s vaccine developed by two Turkish immigrants … Moderna’s vaccine developed by a black woman virologist … Another reason for diversity in STEM … It makes science better.” Of course, STEM being science, technology, engineering an mathematics.
DR. KRISHNA UDAYAKUMAR: Without a doubt.
AMY GOODMAN: Although, actually, that’s our next guest’s tweet. But you can comment on it, on what that means.
DR. KRISHNA UDAYAKUMAR: Sure, without a doubt, I think we have to celebrate also the diversity that allows us to bring the best minds and the most diverse perspectives together that allow us to do the best team science.
AMY GOODMAN: Well, I want to thank you so much, Dr. Krishna Udayakumar, founding director of the Duke Global Health Innovation Center, principal researcher for their project tracking COVID-19 vaccine purchases around the world, practicing physician at Duke University.
Next up, we will be joined by the man who tweeted that issue of diversity in STEM, and that’s Dr. Ashish Jha, dean of the Brown University School of Public Health. Stay with us.









Media Options