
Guests
- Mohga Kamal-Yannipolicy adviser to the People’s Vaccine Alliance and to UNAIDS, the joint U.N. program on HIV and AIDS.
- Achal Prabhalacoordinator of the AccessIBSA project, which campaigns for access to medicines in India, Brazil and South Africa.
While the United States, Britain and other wealthy countries race to vaccinate their populations against the coronavirus, a new report finds that as much as 90% of the population in dozens of poorer countries could be forced to wait until at least 2022 because wealthy countries are hoarding so much of the vaccine supply. A growing movement is calling for the development of a people’s vaccine and the suspension of intellectual property rights to expand access. We speak with Dr. Mohga Kamal-Yanni, a policy adviser to the People’s Vaccine Alliance, and Achal Prabhala, a public health advocate and coordinator of the AccessIBSA project, which campaigns for access to medicines in India, Brazil and South Africa.
Transcript
AMY GOODMAN: President-elect Joe Biden pledged Tuesday to distribute 100 million vaccine shots in the first 100 days of his administration. Biden’s vow came on the same day Britain began a mass vaccination program using a vaccine developed by Pfizer-BioNTech. The vaccine is expected to be soon approved in the United States, as well, as early as tomorrow.
On Tuesday, President Trump held what he called a vaccine summit at the White House. Trump claimed COVID deaths and hospitalizations would quickly decrease, but the White House Coronavirus Task Force is warning the spread of COVID would not be reduced until the spring, based on current vaccination plans. A report by the task force obtained by CNN states, quote, “The current vaccine implementation will not substantially reduce viral spread, hospitalizations, or fatalities until the 100 million Americans with comorbidities can be fully immunized, which will take until the late spring,” unquote.
Meanwhile, a new report finds as many as nine out of 10 people in dozens of poorer countries could miss out on the coronavirus vaccine until at least 2022, because wealthy countries, including the United States, have hoarded enough doses to vaccinate their entire populations nearly three times over. The report was issued by the People’s Vaccine Alliance, which includes Amnesty International, Frontline AIDS, Global Justice Now and Oxfam.
This is Winifred Byanyima, executive director of UNAIDS, in a video produced by the People’s Vaccine Alliance.
WINIFRED BYANYIMA: Huge pharmaceutical companies are keeping the vaccine research a secret. They’re deciding how many vaccines get made, how much to charge for them, and who gets vaccinated. This will no doubt leave billions of people behind. Pharma companies are putting profit, not people, first. Yet billions of dollars of taxpayers’ money is funding their work. We cannot let the CEOs of a handful of pharmaceutical companies decide our future. We need a vaccine that everyone can have free of charge, no matter where you live or whether you are rich or you’re poor. We need companies to share all their research so we can make enough safe vaccines for everyone. We need a vaccine owned by all of us. To end this COVID-19 pandemic, we need to pull together once more.
AMY GOODMAN: That was the UNAIDS executive director, part of the People’s Vaccine Alliance. The World Health Organization has also warned about the inequitable distribution of the vaccine. This is WHO Director-General Tedros Adhanom Ghebreyesus.
TEDROS ADHANOM GHEBREYESUS: We simply cannot accept a world in which the poor and marginalized are trampled by the rich and powerful in the stampede for vaccines. This is a global crisis, and the solutions must be shared equitably as global public goods, not as private commodities that widen inequalities.
AMY GOODMAN: We’re joined right now by two guests. In Oxford, England, Dr. Mohga Kamal-Yanni. She is policy adviser to the People’s Vaccine Alliance and to UNAIDS, the joint U.N. program on HIV and AIDS. She has worked for decades on access to medicines and healthcare in developing countries.
And in Bangalore, India, Achal Prabhala is with us, coordinator of the AccessIBSA project, which campaigns for access to medicines in India, Brazil and South Africa. He recently co-authored an op-ed published in The New York Times headlined “Want Vaccines Fast? Suspend Intellectual Property Rights.” We’re going to begin with the doctor, Dr. Mohga Kamal-Yanni.
You’re in Oxford, actually, where one of those vaccine tests has began, and that is AstraZeneca-Oxford. But start off by talking about what is a people’s vaccine and what are the inequities right now. Who will get this vaccine, what countries, and what countries won’t?
DR. MOHGA KAMAL-YANNI: Well, the People’s Vaccine is a coalition of organizations like Amnesty, Frontline AIDS, Global Justice, Oxfam. It’s co-led by Oxfam and UNAIDS. And it has so many people, you know, academics, health activists, health experts, NGOs, patient groups, from all over the world, united for one aim, which has a people’s vaccine, not a profit vaccine. So we want a vaccine — basically, we’re calling for vaccination that is available for all people at risk, and then for everybody once we have enough doses, but not the way it’s happening now, where if you happen to be born in a rich country, you get the vaccine; if you happen to be born in a poor country, you don’t.
And yesterday in the U.K., they started vaccinating older people, and there was some clapping. And, you know, it was a lot of joy. And, of course, it’s brilliant, you know, that there is hope that this problem that we’re all suffering from will be — you know, there’s a light at the end of the tunnel. However, that joy is only limited to people living here. I’ve got friends and relatives and people that I work with in other countries, in developing countries, who are saying, “Yeah, and what about us?” And yeah, what about them?
So, this is really a big problem. There’s just so many — it’s kind of dividing the world between those who have and can pay and those who don’t and can’t pay, and, therefore, well, you can stand in the back on the queue; we don’t know when you can get the vaccine. And that is just not right. It’s not right on moral grounds. It’s not right on public health grounds, because everybody is saying, “Nobody is safe until everybody is safe.” Yeah, OK. How do you make everybody safe? So, a vaccine nationalism will not get you to everybody safe.
And also, on economic ground, you’re not going to get the economy growing, if just one — or back to normal, if one country vaccinate its population and the rest of the world isn’t. You can’t trade with people who are sick or people who have a high level of infections. So, you know, it just doesn’t make sense at all.
The other important point is that this is not kind of fact of life that, oh, we have limited amount of vaccines. Actually, that’s not the case. There are other options that will enable the world to produce more vaccines, and therefore vaccinate more people. So, basically, what’s happening now, if you can imagine that we have a small pie — so that’s one vaccine, a small pie. And so, basically, the rich can have the bigger share of it, and then we’ll have just crumbs left for developing countries. Well, the idea is that: Well, why don’t we increase supply so everybody can have a decent share of it, rather than fighting on a little one?
JUAN GONZÁLEZ: Well, Dr. Kamal-Yanni, I wanted to ask you about the AstraZeneca-Oxford vaccine and how access to that vaccine may be more equitable at this stage. Could you talk about some of the agreements that the AstraZeneca has reached with the Coalition for Epidemic Preparedness Innovations and Gavi, the Vaccine Alliance?
DR. MOHGA KAMAL-YANNI: Well, basically, I mean, this vaccine has been developed by Oxford University. Oxford University has a standard on managing intellectual property. And it actually talks about open license. However, when they did the deal or the contract with AstraZeneca, it became exclusive license for AstraZeneca. But they managed to put some conditions in the contract about making the vaccine accessible to developing countries.
So, AstraZeneca went to one of the big vaccine producers in India, the Serum Institute, and made an agreement to produce 1 billion doses, so that’s vaccinating 500 million people. Half of them will be in India. So, it’s a good way — you know, good start to make more vaccines available. They also — AstraZeneca also has some agreements with other countries, like with Argentina and Brazil, so that may cover a number of people in Latin America. But what about the rest of the population? There are some other deals with countries, but not production as such.
You know, you can’t leave — you know, so, AstraZeneca, compared to others, yes, they’ve done good things and also fixing the price as — well, AstraZeneca said $4 per dose, and Serum said $3 per dose. For developing countries, it will be probably $3 per dose, so $6 per course or per person. But the thing is, you can’t leave — this is the whole — you can’t leave the decision on supply, price, which country, which patient, to companies. That’s not their job. Their job is to produce. And the job of governments is to make more production, so you have to enable other producers. Like in India, there’s other producers. Other countries would have other producers.
So, if you allow technology transfer, so sharing technology — which the technology, by the way, a lot of it has been developed by public money, including from the U.S. and the U.K. and Europe and other countries. So, allowing the sharing of technology and removing the intellectual property barrier, so no patents on vaccines, then other companies can produce the vaccine, and we have more. And just like AstraZeneca did this contract with Serum, that includes, presumably, technology transfer, or some technology transfer, that can be done on a multilateral level, on a bigger level for more companies. Because all these deals, by the way, they’re all secret. You don’t know what’s in it except what they announce, rather than if you have a multilateral agreement, you don’t — you know, the negotiation happens in closed doors, but then, once they agree a license, then it’s public. Then you see what’s good and what’s bad about it.
JUAN GONZÁLEZ: And what about the whole issue that many developing countries are relying on the possibility of an effective vaccine coming from China? And China, obviously, is in last-stage clinical trials for several vaccines. The potential for China being the one that supplies the bulk of the vaccines to the majority of the people of the planet, what that would mean in terms of international relations in the future?
DR. MOHGA KAMAL-YANNI: Well, I mean, China has four vaccines in clinical trials phase 3. Actually, the Emirates today announced that one of these vaccines passed clinical trials, and they authorized it to work in their country. They were convinced with the safety and efficacy of the clinical trials. So, yes, if developing countries have nothing coming, you know, they can’t just sit — and I heard from a number of countries: “We’re not going to sit and wait.” So they are talking to companies in Europe and in America, but they’re also talking to companies in China. And the king of Morocco said that he’s going to vaccinate his people, and they’re aiming at vaccinating 80% of the population. And again, they have an agreement with a Chinese company. You know, that put the pressure on ensuring that these vaccines have high efficacy and high safety level, or, you know, at least acceptable safety level.
And the thing is, we need that all clinical trials get published, whether that’s from China or Pfizer or Moderna. It’s no good that companies announce their results in a press release to investors, so they have more — you know, their share value and their market value increase, but scientists, who are waiting, who understand these things, cannot investigate or review the results because there’s nothing published for them. So, we need more of transparency on that, including the Chinese, so that countries are aware of what they’re buying.
AMY GOODMAN: I wanted to bring Achal Prabhala into the conversation, again, coordinator of AccessIBSA project, which campaigns to access medicines for India, Brazil, South Africa. This piece you recently wrote in The New York Times, “Want Vaccines Fast? Suspend Intellectual Property Rights.” You’re joining us from Bangalore, India. Can you talk about what that would mean, if you suspended intellectual property rights? Talk about trade secrets. Talk about patents. Talk about government subsidies of these private companies. And how does what’s happening now, the development of this vaccine, compare to people’s access, for example, to the flu vaccine, how that was developed and financed?
ACHAL PRABHALA: Thank you, Amy, firstly. It’s great to be here. And thank you for having me.
The piece that we wrote in The New York Times was geared around an event that’s unfolding this week and the next. It doesn’t look like it will get resolved anytime soon or successfully, but that event is a proposal that South Africa and India made at the WTO, at the World Trade Organization, to temporarily suspend a trade rule called TRIPS, which is an agreement on trade-related aspects of intellectual property, the supergovernance of intellectual property worldwide, which the WTO takes up. And the reason India and South Africa suggested that all member countries of the WTO should be exempted from provisions of TRIPS is so that everything that we require to survive the pandemic — the masks, the test kits, but now especially the vaccines — should be free to be made in as much capacity as possible to get them faster and cheaper to as many people as we can around the world.
There is an overwhelming support from developing countries for this proposal, but the WTO works on consensus, which means that even if five or six very rich countries oppose the proposal, it actually won’t pass. And that’s exactly what’s happening. The U.S., the EU, the U.K. and a few other rich countries, as well as, inexplicably, Brazil, have opposed this proposal and are stalling it, which means that it’s unlikely to go through without a fight.
Now, the irony of the fight having to take place this week is there’s really good news out of the U.K. There’s also really good news out of science. And personally for me, sitting in India, I wish I could share in that good news with the same spirit of cheer and celebration. I saw a moving interview with a 91-year-old called Martin Kenyon in London, who called his hospital, said, “Hey, I heard you had vaccines.” They said, “Yes, come on over and get one.” He walked over, and he got a Pfizer vaccine, the first dose of a Pfizer vaccine. And he’s looking forward to hugging his grandchildren this Christmas. And it’s a beautiful, touching story.
The problem with that is, that Pfizer vaccine, over 90% of its supplies, until the end of 2021 — so that means for the next 13 months — have been sold out to a handful of rich countries, to the U.S., to the EU and to the U.K. There’s actually no way that anyone in India or anyone anywhere outside these rich countries is going to get their hands on one of these vaccines for love or for money. They just don’t exist outside of very few number of rich countries.
That’s kind of amazing to live through in 2020. I’ve been campaigning for access to medicines for a long time. But my father had COVID. He’s 87 years old. My mother is 72 years old. I definitely would like them to have a vaccine and get one fairly quickly. The prospect of these vaccines being unrolled without any possibility of a majority of the world getting them is genuinely heartbreaking. And that’s the anger that partly prompted that piece.
The irony, of course, is that this is such a dramatically different situation from the 1950s when the flu [sic] vaccine was developed by Jonas Salk, who, of course, famously said, when asked by Ed Morrow about whether he was going to patent his invention — he said, “Hahaha, can you patent the sun?” And it’s a heartbreak — it’s a beautiful — it’s a beautiful moment. It’s a really beautiful moment. And —
AMY GOODMAN: And that was about the polio vaccine.
ACHAL PRABHALA: I’m sorry, that was about the polio vaccine. That’s exactly right. And that’s about the polio vaccine.
The tradition of Jonas Salk, however, does continue with the flu vaccine that we all take. That flu vaccine is developed at a unit of the WHO, which it’s called informally the Flu Network, and formally the Global Influenza Surveillance and Research Systems. It’s a collaborative infrastructure that they’ve set up at the WHO that involves 110 different countries, 130 different laboratories, which pool information on what strains of influenza are circulating in their countries. That information is collated. And every year, for two different flu seasons, in the Northern Hemisphere and the Southern Hemisphere, the WHO then releases what would be called the formula for the flu vaccine, which then anyone anywhere can produce, because it’s completely free of any proprietary intellectual property or monopoly, which means that billions of people have taken it since the 1970s based on this cooperative, shared system of pooling knowledge, as well as finances. And that’s created a very robust infrastructure for the production and consumption of these flu vaccines. And it’s a great success. It’s, unfortunately, exactly the kind of thing that’s not being replicated with the coronavirus vaccines.
JUAN GONZÁLEZ: Well, Achal Prabhala, I wanted to ask you: In terms of the refusal of these handful of rich countries to allow the suspension of intellectual property rights at the WTO, what is their argument? Given the enormous worldwide crisis that we’re functioning, how do they defend this? And what could possibly be done to overcome this resistance?
ACHAL PRABHALA: Juan, that’s an excellent question. And look, I think, in some way, I’ve been debating several people on this just this week, after The New York Times piece came out, as well as previously, because of my work. I wish, actually, sometimes that people would just be honest and upfront and say, “Look, we actually care about these corporations more than global human life. We’re actually fine with a certain number of usually poor people dying for a lack of access to these vaccines, as long as the companies and the industry that makes them survives.” I’d be willing to listen to that argument, because it at least would be honest.
What happens instead is that the arguments that are advanced are, A, that it’s not a problem. To say that it’s not a problem ignores 20 years of human history, where millions of people died because of lack of access to monopoly drugs for AIDS, and then did so again for lack of access to drugs for cancer, and then did so again for lack of access to hepatitis C drugs, and, by the way, are doing today in the United States for lack of access to insulin, which is, again, patented, for lack of access to PrEP for AIDS, or for a lack of access to cystic fibrosis drugs in the U.K. So, it’s to deny reality.
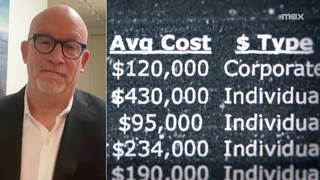
But the logic that’s advanced is that the innovation system requires these monopolies to exist in order to reward private pharmaceutical corporations for taking big risks with private money — except for the fact that that’s not what’s happening here. It’s never happened, but it’s never happened as starkly as it is not happening in the pandemic. Moderna, which is just one of the vaccines that posted successful results a couple of weeks ago, has admitted, by its own — in its own financial reports, that 100% of its vaccine development project was funded by BARDA, by Warp Speed and the U.S. government, U.S. taxpayer money. On top of that, it’s been given preorders of another one-and-a-half billion from the United States and another substantial amount of money, nearing about a billion, from the European Union. Every other vaccine, from Pfizer to AstraZeneca, also has substantial government money. German taxpayer money of up to $445 million went into the Pfizer vaccine. AstraZeneca received huge subsidies through public money from the United Kingdom through its early development at Oxford University. All of these vaccines have, on top of that, received these very lucrative, very large preorders.
Now, you can’t have it all ways. You cannot have a vaccine project literally contracted out — I hesitate to say “subsidy,” because when it’s 100% of the cost, that’s not a subsidy, that’s ownership. You cannot have a price like a preorder of $6 billion, which is basically what Pfizer has awaiting it on successful completion of its trials and approval, and, on top of that, say, “But we also need the intellectual property monopoly because of all this private capital we’ve risked,” which doesn’t seem to actually exist. It is very, very strange, but this is the argument that’s being advanced, and it doesn’t hold water. I think they understand that, as well. It’s just that this argument has a rich history. It’s embedded in a particular kind of thinking, a particular branch of economics, which they know that they can ride on and, in effect, lie their way through opposing what is really a very sensible and unradical proposal made by South Africa and India at the WTO.
AMY GOODMAN: So, finally, how exactly — summing up in a minute, if you got around trade secrets, if the companies were forced to release their trade secrets, they didn’t get patents on this, how would a people’s vaccine work? Every company all over could just develop the vaccine where it is? What’s shocking, President Trump signs some executive order, not clear how enforceable it is, called “America First.” We have learned, if you’re altruistic or not, if someone is sick somewhere in the world, you are in danger. So, this is — everyone is in this together. But what would a people’s vaccine — how would it happen?
ACHAL PRABHALA: What it requires is, firstly, for companies to say, “There are two aspects of our monopoly that we’ll give up. We will share with you our patents, and we’ll share with you our trade secrets.” Trade secrets are the know-how and the technology that’s required to make a vaccine. It’s a very important part of the process. If they were to say, “Look, we’ll license this to any company with a reputation and a quality certification that’s willing to make this vaccine with us,” then let’s open it up, and let’s have anyone interested do it. And if they did that, they would suddenly find that there are whole avenues of supply that open up around the world. There are over 20 vaccine manufacturers in India, but there are also eight vaccine manufacturers on the continent of Africa. And there are a number of ways in which you can do this collaboratively. The one way not to do it is the way that they are, by producing these artificially limited quantities of these vaccines by sort of keeping it all to themselves.
JUAN GONZÁLEZ: And I wanted to ask Dr. Kamal-Yanni again about the situation with — the Trump administration had removed the United States from the World Health Organization. President-elect Biden is now saying he will return the U.S. to the WHO. What do you think has been the impact of the United States pulling out of the WHO in the midst of this pandemic?
DR. MOHGA KAMAL-YANNI: Well, I mean, what do you say about such an amazing, really incredible, irresponsible, I’m afraid, decision in the middle of a pandemic to do that? I mean, it’s a strange decision even if we’re not in a pandemic. So what do you think if we are in the middle of it? It’s really, really not very good.
My dream, to be honest, as a non-American, about your election, is to retain two things: one, the American role in advancing global health, and particularly in joining the WHO, and also, you know, putting science before politics. This has been also very, very problematic from the U.S. It really affected not just decision makers in other countries, but also ordinary people. This ignoring the science behind COVID was really, really bad.
So, we do hope that the new administration — I mean, they made commitment — Biden made a commitment to join the WHO. That is fantastic. The sooner, the better, you know? That would be great, but also for the U.S. to join something like or to voice public support for something like this technology access pool that WHO and other countries co-sponsored to do the facilitation of licensing intellectual property and — so, managing intellectual property — you know, your previous question — but also facilitating technology transfer to other companies. So, supporting the C-TAP would be absolutely fantastic.
For the U.S. new administration, I mean, it’s not in — it wouldn’t catch that December meeting that my colleague was talking about, but, in general, playing a positive role in the WTO in putting public health before profit. And we’re not saying companies don’t make profit. We’re not saying that at all. But we’re saying that public health comes before profit, which is, by the way, something that all the World Trade Organization members agreed on in Doha in 2001. So, it —
AMY GOODMAN: Dr. Mohga Kamal — we want to thank so much for being with us, Dr. Mohga Kamal-Yanni, People’s Vaccine Alliance and UNAIDS. And thank you to Achal Prabhala, the AccessIBSA project, co-authored New York Times headlined piece, that we will link to, “Want Vaccines Fast? Suspend Intellectual Property Rights.” He’s speaking to us from Bangalore, and the doctor is speaking to us from Oxford, England.
When we come back, we look at why former jurors and even a prosecutor are speaking out against the federal execution of an African American man, Brandon Bernard, scheduled to die Thursday — on International Human Rights Day. Stay with us.










Media Options