
Despite strong objections of public health officials, governors in Georgia, Tennessee and South Carolina still plan to reopen parks, beaches and nonessential businesses. Even Trump reversed his support. Increased testing is critical for the whole country. But where are the tests? We look at the path ahead with Dr. Syra Madad, infectious disease specialist and special pathogens expert, who was recently featured in the Netflix docuseries “Pandemic.”
Transcript
AMY GOODMAN: Well, we are broadcasting from New York City, where the COVID-19 death toll has passed 15,000. The number of daily deaths has finally begun to decrease, after more than a month of strict social distancing. Officials warn there is still a long road ahead for New York’s recovery. Increased testing will be critical as New York City and other localities look to slowly reopen certain parts of society.
New York Governor Andrew Cuomo met with President Trump in Washington on Tuesday to discuss federal aid for expanding testing capacity, and said the president committed to helping New York state double both its COVID-19 and antibody tests to 40,000 a day. But Wednesday, Senate Majority Leader Mitch McConnell said he’s against giving states more federal aid in future pandemic legislation, suggesting states should instead consider filing for bankruptcy. Governor Cuomo called the statement “one of the saddest, really dumb comments of all time,” unquote.
This all comes as the governors in Georgia, Tennessee and South Carolina are preparing to reopen parks, beaches and nonessential businesses despite the strong objections of public health officials. Last weekend, President Trump encouraged far-right anti-quarantine protesters — many of them openly brandishing assault rifles — tweeting they should “liberate” Michigan, Minnesota and Virginia. But on Tuesday, Trump said he disagreed strongly with Georgia Republican Governor Brian Kemp’s decision to reopen businesses.
PRESIDENT DONALD TRUMP: The spas and the beauty parlors and barber shops, tattoo parlors, I love ’em, but they can wait a little bit longer, just a little bit, not much, because safety has to predominate. We have to have that. So, I told the governor, very simply, that I disagree with his decision, but he has to do what he thinks is right.
AMY GOODMAN: Meanwhile, the head of the Centers for Disease Control and Prevention has warned a second wave of the coronavirus could hit the U.S. in the winter with even more devastating results.
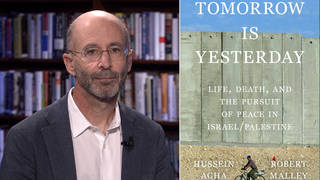
For more, we’re joined by Dr. Syra Madad, an infectious disease specialist, special pathogens expert, here in New York City. She was recently featured in the Netflix docuseries Pandemic, which premiered in January.
Welcome to Democracy Now!, Dr. Madad. It’s great to have you with us. Why don’t we start off with what seems to be, to the shock of many, this controversial issue of testing? How is it possible in the United States that we are still at the point where just last week a 92-year-old woman, the mother of our co-host Juan González, went to a top hospital in New Jersey, 92 years old with COVID symptoms, and she was told she could not be tested? Only when they finally agreed to admit her did they say, well, then they had to do a COVID test to decide which wing to put her in. But that is one of many, many examples, the lack of access that governors, that people in general all over the country, have to tests. Why is testing so important?
DR. SYRA MADAD: It’s a great question. Everyone’s asking that: Why testing is so important? And I’m sure many people keep hearing about, you know, ramping up testing. And the reason why testing is so important, not only to know that you actually are infected with coronavirus disease, while probably clinical management won’t change much, unless you’re in the high-risk group and require additional services, but it’s also extremely important to know you’re positive, so that way we can isolate you, and so you don’t start new chains of transmission.
And unfortunately, here in the United States, we’ve almost seen a — hit a plateau when it comes to testing. We’re not really increasing the number of testing being done yet, for a number of different reasons. One big one is because of the whole supply chain aspect, because there’s not enough of the reagents and the swabs that are needed to actually conduct the testing. A lot of states actually have the infrastructure to do the testing, but really it’s relying on the supplies itself, that unfortunately is just not there yet.
And so we really need to make sure we have widespread testing and a good infrastructure in place. That way, we can test anybody that needs it. So, you know, if you’re symptomatic, even if you’re asymptomatic, we want to make sure that we have a test available to be able to see whether you have coronavirus disease, because the biggest thing is we want to make sure that you’re able to isolate yourself so you don’t start these new chains of transmission and infect additional people. This is, you know, a very highly transmissible virus that’s proven to be quite lethal, if you will. So we need to really make sure that we have these systems in place in order for us to really open back up, if you will.
NERMEEN SHAIKH: And, Dr. Madad, could you explain what the different kinds of tests are that are being carried out? Are they all the same across the board? What, for example, is the distinction, the difference, between an antibody test and a test to determine whether you have COVID-19 right now? Are they the same? And you talked about the problem with supply chains. Where is the material being produced for these tests? And is there any likelihood that their production could be expedited now and continue to be 'til they're needed?
DR. SYRA MADAD: So, in terms of testing, there is an antigen test that looks for acute infection, meaning if you’re actually infected with coronavirus disease, it actually looks for the virus itself through molecular assay. And then the other test is the antibody test, or the serology test, that actually looks to see if you had the infection previously and have developed an immune response. It’s actually looking at the antibodies in your blood. So, there is two very distinct means. One could be used for diagnostic purposes, if you will, the antigen test.
The antibody test is something that is relatively new, and I would highly caution anybody using the serology test right now to make any type of decision. And the reason why I say that is because the assays that are being used for serology tests, so the serology test itself, the blood that is drawn and tested, is very hard to interpret the information. First, the testing itself, you’re getting a lot of false positives, false negatives. It doesn’t seem to be — depending on the type of test you’re using, you know, a lot of these are not validated and not going through a quality control measure. We can’t see if they’re providing true results.
And the other big issue when it comes to serology is — and I think it’s very important for people to state — we just don’t know a whole lot about this virus. There’s still a lot of the science that we do not know. We don’t know about the pathophysiology of coronavirus disease. And so, even if, for example, you may have a positive antibody test, what does that mean? Does it mean that you are actually immune to coronavirus disease, you can’t get reinfected? We don’t know that. We don’t know how much — you know, the titer level that you need that will actually confer immunity. We actually don’t know that. There needs to be a lot more data on that. And on top of that, we also don’t know the risk, as I mentioned, of reinfection. And so, these are things that I think we need to be very public about. This is the science that we don’t know, that we hope to know in the future. It’s not there yet. This is a puzzle that is missing a number of pieces. And so, while we want to rely on seroprevalence and conducting serosurveys and seeing how many people are actually immune, we really need to take that with a grain of salt, because, again, we don’t know a lot.
AMY GOODMAN: So, Dr. Syra Madad, I wanted to ask you about this possibility of how you open the country — what President Trump is pushing so hard for, has been saying that these gun-toting activists around the country who are demanding their states open, are liberating their states — what a rational plan would be. I wanted to ask what you think of the Rockefeller Foundation plan that’s just put out there. Paul Romer, the Nobel Prize-winning economist, has recently said some very interesting things. I mean, they’re calling for 30 million tests a day in the United States, so that people — a day in the United States. He’s calling for a day. The report, I think, is calling for 30 million tests a week. He said it should be a day. I think he compared it to that the U.S. makes something like 350 million cans of soda a day — why can’t we do 30 million a day? The report itself, though, calling for 30 million a week. We are so far from any of that. I think that would clearly go to the issue of the Defense Production Act, President Trump demanding that companies start to convert to making these tests. Trump has been extremely resistant to this idea of mass testing. But how else do you open the country without having to shut it down right away because there’s another mass outbreak, because workers come together who are both positive and those that weren’t exposed?
DR. SYRA MADAD: You’re absolutely right. And I think the best way to really show the American public, you know, what situation we’re in is look at where we’re at right now, right? One of the reasons why we’re seeing a decrease in the number of cases, depending on where you are, if you’re at least in the state of New York, is because of our collective actions, doing what we call social distancing, physically distancing ourselves. And the reason why we’re doing that is because we want to obviously make sure that, you know, we’re not going out, we’re not coming in contact with the virus. Right? So, the endgame is, the whole goal is making sure we don’t come in contact with the virus, because if you come in contact with the virus, then, obviously, you can get infected. And right now no one has, really, immunity to this virus, because this is brand new, unless, obviously, you’re already going through active infection right now. And so, the virus is still out there. And one of the reasons why we’ve been able to decrease the number of cases is because of social distancing.
If you take that away, that very effective public health measure, then we’re going to be in the same position that we were back in January, back in February, back in March, because nothing has changed between now and then. We still don’t have enough testing. And we still don’t have, you know, a testing — a treatment option yet. And then we have clinical trials still in the pipeline. People are actually getting very confused, I think, in terms of when we’re talking about all these different medications. I think some people, when I’ve been talking to them, they think these are cures. These are not cures. There is no cure for coronavirus disease. There are a number of different treatments that are in clinical stages. How effective and safe they are, that’s still something that’s being explored. And so, nothing has changed. And if we are to reopen the economy, being in the same position that we’re going to put ourselves in, we’re obviously going to see a resurgence of cases.
And as we’ve seen with history — right? — a lot of people have been comparing this to the 1918 Spanish flu — the second wave was much higher and much more severe than the first one. And so, if we’re going to let history repeat ourself, I think we just need to make sure that we’re prepared for it. And unfortunately, we are not.
And I think the other thing we need to also think about is how do we define risk and how do we define the word “safe,” because that’s — you know, living with COVID-19 is going to be our new normal, so we need to make sure what amount of risk are we able to take, if at all. And what does that word “safe” actually mean? We’re not going to really be safe. As long as that virus is out there and lingering, we’re not going to be safe. So we need to continue to do various public health measures really to protect everybody.
NERMEEN SHAIKH: Dr. Madad, that’s a very good point that you make about how essential social distancing is, given where we are now with both testing and clinical trials for drugs. Could you give us some sense, because obviously the costs of social distancing and the impossibility of social distancing in a large part of the world, the developing world, in particular, and in poorer — among poorer communities everywhere, where it’s simply not possible to be socially distant from others, what — how far are we along in clinical trials? And are there any alternatives at all to social distancing at the moment or in the foreseeable future, the near future?
DR. SYRA MADAD: So, any of these potential treatments that are being studied, they’re not going to be a silver bullet. And what I mean by that is they’re not going to be 100%. We still are waiting on the data for a number of these different pharmaceutical interventions to come out. You’re seeing some come out right now. For example, you know, hydroxychloroquine, you’re seeing whether it’s safe and effective, and in fact the data is showing otherwise, that it actually is not effective. And then you’re seeing other studies come out with remdesivir, that is showing — that is looking promising.
But again, you know, when you’re doing these clinical trials, you really need to go through the proper channels and making sure that you’re studying these individuals for a longer period of time. And that’s obviously not happening right now. These are very quick, short studies. And so, I think, in the coming weeks to months, we’ll probably get some more information in terms of the various clinical trials that are out there around the world, not just here in the United States. And so, you know, it seems as if we’ll —
AMY GOODMAN: And, Dr. Madad —
DR. SYRA MADAD: Yeah.
AMY GOODMAN: Do you want to weigh in on this huge controversy that’s happening with Dr. Bright right now? I mean, President Trump, the Trump administration, fires the person in charge of vaccines in the government, who has been fighting hard to coordinate all these kind of tests you’re talking about, clearly opposed to, you know, prescribing hydroxychloroquine or chloroquine without the proper studies, and now being taken out as he resists President Trump’s drug of choice, which hasn’t even been adequately tested.
DR. SYRA MADAD: You know, this is something I’ve been saying from the get-go. We really need to let science speak, and we really need to look at the facts. We need to follow the facts. There is, obviously, a lot that we don’t know, and we need to be very clear about that. And we need to make sure people understand. When we don’t know something, we’re providing that information; when we do know something, we can provide that information. And, you know, doing these types of — and having these types of actions and reactions is very unfortunate, because, really, it’s showing the credibility of the administration in and of itself. And this is a very pressing time, and a lot of lives are on the line. And we really need to make sure that we’re following the facts. And so we want to make sure that we are having experts be able to be at the table and drive these conversations.
AMY GOODMAN: We want to go to a break, and then we’re going to come back to Dr. Syra Madad, infectious disease specialist, special pathogens expert, here in New York City and for New York City. We’ll be back with Dr. Madad in a minute.
[break]
AMY GOODMAN: “Oh, What a World 2.0” by Kacey Musgraves. She reworked her song from 2018 and released it Wednesday on the 50th anniversary of Earth Day. This is Democracy Now!, democracynow.org, The Quarantine Report. I’m Amy Goodman, with Nermeen Shaikh. We’re both in the epicenter of the pandemic, as we continue to look at the path ahead for this pandemic, how we respond, how we consider when to reopen, with Dr. Syra Madad, infectious disease specialist, special pathogens expert. Dr. Madad, if you could talk about your own personal experience? Did you test positive for COVID-19?
DR. SYRA MADAD: Well, I did. I did test positive for COVID-19. Certainly, I think anyone getting that type of test result, it is scary, especially knowing, you know, if you have loved ones at home, those that are even in the high-risk category, which, for me, I do. It was something that, you know, when I got the test result, wasn’t surprising, really, unfortunately, given the circumstances and being out there. But I was able to quickly isolate myself. And luckily, everybody in my household was able to recover.
One of the symptoms that I had was the loss of taste and smell. And I actually had that for quite a few weeks. And just, actually, as of recently, I was able to get my full taste and smell back and be able to enjoy, for example, my cup of coffee. But, you know, with the coronavirus disease, the spectrum of illness is so wide and variable. You have people that are asymptomatic. You have those that have mild signs and symptoms of the disease. And then you have those that are more severe and critical, and people falling on those buckets. You know, right now we know there are certain aspects that put those in the high-risk category, but you’re also seeing very young, healthy individuals fall anywhere on that spectrum.
So, again, don’t know a whole lot about this disease, but we’re hopeful that as the days and hours and weeks progress, that we can learn more through, you know, factual means. And when I say “factual means,” you’re seeing a lot of information come out, a lot of things being published, not going through peer review. So, I caution anybody that’s going through a lot of — in reading a lot about this, making sure that you’re reading peer-reviewed information, things that actually have been going —
AMY GOODMAN: Dr. Syra Madad —
DR. SYRA MADAD: Yes.
AMY GOODMAN: Before we talk about that kind of information, just your own is so important for people to see someone who has recovered from COVID-19. You have three kids, right? Your last child, you just gave birth to in January? Can you talk about the kind of decisions you had to make when you tested positive, and what it means to isolate for a mom like you and a new mother?
DR. SYRA MADAD: So, you know, as you mentioned, I actually delivered in January my youngest. My baby girl turned 3 months most recently. And I’m a breast-feeding mother, 100%. So, it was certainly difficult, you know, to be able to isolate myself from my children, knowing I potentially already exposed them, after I had gotten my test results, because from what we know, you can actually spread the virus before actually being symptomatic. So everybody was already exposed in our household. And as I mentioned, luckily, everybody recovered. But, for me, as soon as I became symptomatic, I did isolate myself for a period of time, until I was afebrile for at least 72 hours. Certainly had a big impact on my family. Luckily, I have a great support system. My husband was able to watch the kids. But at the same time, I knew he obviously had it, as well. But I was symptomatic. Then —
AMY GOODMAN: He had it, too? He was positive, as well?
DR. SYRA MADAD: He had it, too, yeah. He was symptomatic first, and then I became symptomatic. And so, when I did, I was able to isolate myself, and he was not symptomatic during that time. But, you know, we had already exposed our children, if you will. And luckily, they actually had very mild signs and symptoms. We didn’t get them tested. The only person that actually did get tested is myself, as a person working in a healthcare system. And my in-laws, actually, both high-risk, one actually on hospice care, he actually did also get tested and did get tested positive. But we’re very lucky that everybody was able to recover.
NERMEEN SHAIKH: Dr. Madad, you mentioned that the spectrum of illness is so wide with COVID-19. And obviously, we’re all just learning about how this disease, this virus, spreads. But is there anything that can predict how severe the illness will be in people who get it?
DR. SYRA MADAD: That’s an excellent question. And what we’re seeing right now is, while we know this virus can infect anybody and anyone, if you will, regardless of your age, regardless of your health status — you know, this is just one of those viruses. You know, we know that it’s ubiquitous. But at the same time, there are these health disparities and social determinants that may put you at even high risk for having a worser outcome. And we’re actually seeing some of this play out. So, for example, you’re seeing a higher rate of infection in the African-American community. You’re seeing a high rate of infection in the Latino community.
And I think when you look at some of the social determinants of health, you’re also looking at the socioeconomic status and some of those variables that actually may put them at higher risk because of the type of work that they’re doing, for example, as essential workers, also looking at their living conditions, living in close quarters. I think it was by no accident that one of the first hospitals that was overwhelmed in New York City was Elmhurst Hospital. The reason for that is that particular area and that ZIP code is one of the most diverse urban areas in the United States, and you have a lot of families living together in close corridors.
And so, when we talked about social distancing, and as we mentioned actually earlier, you know, some people don’t have the privilege of actually socially distancing themselves, because there are so many people living in their household. And so, because of that, you can spread the virus much more easily and quickly. And we’re seeing a lot of that play out.
AMY GOODMAN: And can I ask you about this new observation? Not really new among the docs all over the country. I had gotten this random text last week: It’s not about the pneumonia, it’s about the blood clots. And I wanted to read to you from a Washington Post piece, “A mysterious blood-clotting complication is killing coronavirus patients.” It says, “Increasingly, doctors also are reporting bizarre, unsettling cases that don’t seem to follow any of the textbooks they’ve trained on. They describe patients with startlingly low oxygen levels — so low that they would normally be unconscious or near death — talking and swiping on their phones. Asymptomatic pregnant women suddenly in cardiac arrest. Patients who by all conventional measures seem to have mild disease deteriorating within minutes and dying at home.” And they’re saying it seems to be this issue of blood clots. In fact, the first person now, who’s believed to be weeks before we really believed, a 57-year-old woman in California, who was in very good shape, no preexisting conditions, it looks like she also died in this way, of sudden maybe cardiac arrest, and people didn’t identify it as coronavirus in the beginning of February. What about this blood clotting issue?
DR. SYRA MADAD: It certainly is an issue. And from what we’re seeing, you know, what hospitals are reporting, it is becoming — and I wouldn’t say “becoming” — it does seem to be a common issue. But what we’re also seeing is that, you know, while maybe folks may think that COVID-19 is more implicated with the lungs, we’re actually seeing a number of different organs within the body actually in distress and having various manifestations. So you’re seeing issues with kidneys and heart and brain and liver. And so, the way that it can manifest is obviously very different, and it depends on the individual, their immunoresponse and the body response.
But what we also don’t know is the sequelae. And what I mean by that is the long-term effects of COVID-19. And this is something — as I mentioned, it’s a new virus. It’s only about 4 or 5 months old. And we’re learning a lot about it, and a lot we don’t know. And everyone is really learning at the same time. We’re relying on each other to be transparent and show data and share some of the case studies that we’re seeing, that may help others that are obviously treating individuals with COVID-19.
But, you know, I think a good example would be, for example, Zika. You know, Zika was relatively something that a healthcare system did not experience that in the magnitude that we did a few years ago. And you saw, obviously, children being born with microcephaly and having other issues. Those individuals, those children, are still being studied long-term to actually look at the full effect of Zika. And you’re still seeing data come out.
And similarly with COVID-19, this being a new virus in and of itself, it’s going to take years for us to actually see the long-term effects, because we need to follow these individuals for their entire lifetime to actually see, you know, does it have additional effects on them, not just during the acute stage when they’re actually infected and in the hospital, but also once they get discharged. Is it going to have any effect on their health, moving forward? And really, that’s a question that we don’t have an answer to yet.
NERMEEN SHAIKH: And, Dr. Madad, very quickly, before we conclude, as I’m sure you know, many people are relying on the development of a vaccine, even if it will take from 12 to 18 months. But you’ve said that even a vaccine won’t be a silver bullet, as you said. Why is that? And what about your concerns about certain people perhaps not getting the vaccine even once it’s available? Why would people do that?
DR. SYRA MADAD: Well, first, I think when we say 12 to 18 months, you know, that is an optimistic timeline. Is it realistic? I don’t think it is very realistic, knowing that developing a vaccine actually takes years and years. And we really need to be very careful in making sure that we’re having a safe and effective vaccine to actually administer to the American public and globally.
And I think once we do have a vaccine that is safe and proven to be safe and effective, and whenever that will be, we’re going to have to jump through additional hurdles, like those that are hesitant to actually get vaccinated. You know, as you may be aware, the anti-vax movement is vast. It actually is one of the biggest — one of the biggest global health problems that we have in the world. So we need to make sure that even once we have a vaccine available, people are actually able and less reluctant to actually get vaccinated. But even on top of that, when these vaccines are manufactured, not everybody is going to get the vaccine at the same time. There are going to be — there’s going to be a short supply. And to get everyone vaccinated will take years. You know, we’re a very, very large country with many individuals. And to be able to vaccinate everybody that is eligible to get vaccinated will take at least a year or two, or maybe even longer. And so we need to really face the facts and know that this is where we’re at, and we know that there’s going to be additional hurdles once that vaccine is available. And so, this whole notion of herd immunity, and so on and so forth, we really need to give it a lot more thought.
AMY GOODMAN: Well, we want to thank you so much, Dr. Syra Madad, infectious disease specialist, special pathogens expert, featured in the first episode of this remarkable series that came out on Netflix called Pandemic, which, unbelievably enough, came out right at the beginning. And, Dr. Madad, we’re so thankful that you and your family now are safe, are healthy, and we just hope that for the rest of the country and the world.
We also have this breaking news: The Labor Department has just reported another 4.4 million people, U.S. citizens, filed for unemployment claims over the last week, bringing the total over the past five weeks to over 26 million. That doesn’t even include the millions of undocumented immigrants living in the U.S. who have lost their jobs due to the pandemic, and those who tried to apply but weren’t able to.
When we come back, we speak to another doctor, a global health expert, about the efforts to stop the daily spread of COVID-19 with contact tracing in Massachusetts — following those who have been in contact with those who have COVID-19. Stay with us.
[break]
AMY GOODMAN: “He Will See You Through,” sung and written by Rhiannon Giddens, with Francesco Turrisi on accordion — they are social distancing in two different places — as part of the Humanity in Concert series.










Media Options