
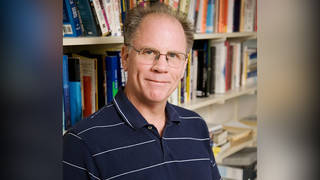
We speak with Dr. Richard Levitan, an emergency physician based in Littleton, New Hampshire, who volunteered at Bellevue Hospital in Manhattan for 10 days at the height of the COVID-19 surge in April. Based on what he saw, he argues patients should be going to hospitals sooner and that medical professionals could use a small device you clip on your fingertip, called a pulse oximeter, to help detect the virus earlier by revealing oxygenation problems and elevated heart rates. “A pulse oximeter is just a measure of identifying how well the lungs are working, and, I believe, can be basically an early warning system in terms of patients to know who has COVID pneumonia,” says Dr. Levitan.
Transcript
AMY GOODMAN: We turn now to our last segment. This is Democracy Now! The Quarantine Report. I’m Amy Goodman, as we look at the effort to save more lives as the coronavirus pandemic continues to rage across the United States and around the world. Even as President Trump presses states to begin reopening, he predicted Sunday the U.S. death toll from the pandemic could reach 100,000 — a number far higher than his earlier estimate a week or two ago of 60,000.
We’re joined now by Dr. Richard Levitan, an emergency physician who’s usually based in Littleton, New Hampshire, but he came down to New York to volunteer at one of the public hospitals, at Bellevue Hospital, where my dad used to work, in Manhattan, for 10 days at the height of the COVID-19 surge in April. He was shocked by what he saw. He wrote about what he learned in The New York Times op-ed headlined “The Infection That’s Silently Killing Coronavirus Patients.” In it, he writes, “I realized that we are not detecting the deadly pneumonia the virus causes early enough and that we could be doing more to keep patients off ventilators — and alive.”
Dr. Levitan, if you could tell us how exactly you do that? Welcome.
DR. RICHARD LEVITAN: Thank you for having me. For the last 30 years in medicine, we have used a fifth vital sign. So, the standard vital signs of heart rate, blood pressure, temperature, respiratory rate, we’ve added a fifth vital sign. That fifth vital sign is pulse oximetry. And what it does is it measures the saturation of oxygen in the blood. And what I noticed while working in New York is these patients came in with alarmingly low oxygen saturations, but they did not, subjectively, actually feel short of breath.
AMY GOODMAN: So, explain this oximeter. Explain exactly what it is. And interestingly, the inventor of the oximeter, Takuo Aoyagi — an ingenious and indispensable medical device, as many are describing it — just died, and his death was just announced.
DR. RICHARD LEVITAN: Yeah. So, if you’ve interacted with the healthcare system at all in the last 30 years, you’ve had a small probe placed on your finger. In the hospital, those probes connect up to our monitors. But there also now fingertip versions of this. And these devices are very inexpensive, and they are widely available. They are present or ready on every ambulance, in every hospital, in every doctor’s office, actually in every nursing home. They exist widely. And this device gives you two numbers. It gives you a heart rate, and it gives you an oxygen saturation.
And so, what is remarkable about this is that the cause of death in COVID, overwhelmingly, is pneumonia. Pneumonia triggers hospitalization, and often requirements for mechanical ventilation, and then all these problems ensue after the lungs get severely injured. And a pulse oximeter is just a measure of identifying how well the lungs are working, and, I believe, can be basically an early warning system in terms of patients to know who has COVID pneumonia.
AMY GOODMAN: So, describe what doctors all over the country, and nurses, are seeing in hospitals, something that they really haven’t seen before, where someone will be on their cellphone, they’ll be talking to the doctors and nurses, and then suddenly crash. Explain that. And then talk also about your concern about people being put on ventilators. What? At this point, something like 85% of people who have been put on ventilators die?
DR. RICHARD LEVITAN: So, the rate of death on ventilators varies dramatically. And unfortunately, the public has the perception that everybody who gets put on a ventilator dies. It really depends how sick you are on presentation. If you are elderly, if your lungs are terribly involved, you know, your mortality, being put on a ventilator, is high. But among young people, actually, the death rate on ventilators is much lower. So, I don’t want the public to be scared that if their loved one winds up on a ventilator, that that necessarily means a death sentence.
But it is a bad thing when people get COVID pneumonia and they present late. In terms of their presentation, we see all the time in emergency medicine that when people choke, when they drown, anything that affects oxygen going to the brain, when that happens quickly, patients pass out, or they have seizures. The remarkable thing about these patients are they come in with oximetry readings, pulse oximetry readings, oxygen saturation readings, half-normal, as low as 50%. And we normally have an oxygen saturation between 94 and 100. But so, these people are there with these incredibly low readings, and their brain is working fine, and they’re on their cellphone. And what they have done, as an adaptation to this low oxygen caused by the pneumonia, is they have silently kind of increased their breathing rate over days. And they only come in when they get either short of breath or a fever, but that happens late in the process. Subjective shortness of breath is not something that the patients appreciate, because this disease basically silently advances until they get seriously ill.
AMY GOODMAN: And so, you’re saying, when people are told, “Do not go into the emergency room before you have that shortness of breath. Just stay at home,” can be a real problem, that people are holding off to the end, when it could be too late?
DR. RICHARD LEVITAN: Well, looking back on my own experience with COVID before I went to New York, and I was evaluating patients in the hospital, and we were sending out COVID tests, I followed what the CDC guidance was. I told patients, “Let us know if you get short of breath.” There are, in fact, posters from the CDC that say, “Do not go to the hospital if you have a cough or you have shortness of breath. Only go to the hospital if you have trouble breathing, you’re unable to be awoken, or you turn blue.”
Well, in hindsight, what I now appreciate is that a very, very small number of patients have subjective shortness of breath. When they do get short of breath, they’re really ill. So, the public messaging needs to change. The public needs to know that earlier diagnosis, identification that you have COVID, and then monitoring with one of these little devices can warn you about the need to return and be hospitalized. And if you come in earlier, we can do much better treating your pneumonia, identifying how much inflammation there is, getting drugs into you, and other things.
AMY GOODMAN: Dr. Richard Levitan, you were incredibly brave to come from this rural area in New Hampshire to New York, come back to where you grew up, but to Bellevue, a city hospital, to say you want to offer your services. We know the kind of threat you yourself put yourself in, the dangerous situation, and so many doctors, nurses, staffers at hospitals, the people who clean up, are in that kind of situation every day. And yet, when you came to New York to offer your services, can you describe what happened when you found a place to stay, your brother’s apartment, what the building did?
DR. RICHARD LEVITAN: Yeah. So, I got kicked out of my brother’s apartment when they found out I was working at Bellevue. But, you know, let me just say that the people in New York City, the frontline healthcare workers, my friends in emergency medicine departments around the city, you know, they were in this fight for weeks before I arrived. They’re still in this fight now. I spent 10 days. You know, the heroes here are the people who are in this for the long haul. I just —
AMY GOODMAN: But I just want to point out, here we are, based in New York City, in the epicenter of the pandemic. The building, the co-op that your brother is in, they kicked you out because you were a doctor who came in and were working at Bellevue? They said you couldn’t stay there?
DR. RICHARD LEVITAN: You know, so, this pandemic, this virus, has scared a lot of people. And, you know, as it turns out, yeah, that’s what landed me in a story in The New York Times.
But what ended up happening, and over the course of my 10 days, was this amazing transformation in care, that, over time, we learned that a lot of patients with severe COVID pneumonia could actually be managed without ventilators. And that realization actually led me to recontact Jim Dwyer at The New York Times, who had done the first article about me. And he subsequently produced an incredible article, along with Robin Stein, who had an incredible video, discussing what doctors wished they had known a month ago. And what it ended up doing was kind of explaining how dramatically practice has changed. And this is a great message for the public to understand, that —
AMY GOODMAN: We have 10 seconds. Ten seconds. Go ahead, Dr. Levitan.
DR. RICHARD LEVITAN: Right. So, about two out of three patients who we now see with COVID pneumonia, we can manage without ventilators.
AMY GOODMAN: Well, we’ll link to Jim Dwyer’s piece and your own op-ed piece. Dr. Richard Levitan, thank you for coming to New York to help us here. Dr. Levitan is an emergency physician in Littleton, New Hampshire, volunteered at Bellevue Hospital, a public hospital in New York, for 10 days at the height of the COVID-19 surge in April.
That does it for our show. A very Happy Birthday to Denis Moynihan!
Democracy Now! is working with as few people on site as possible. The majority of our amazing team is working from home. I’m Amy Goodman. Thanks so much for joining us. Stay safe.









Media Options