
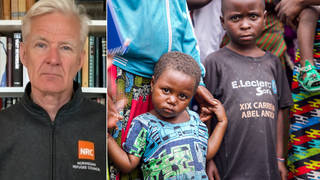
Guests
- David Hayes-Bautistadirector of the Center for the Study of Latino Health and Culture at UCLA School of Medicine.
Amid a surge in coronavirus cases and hospitalizations across the United States, the Latinx community has been hit especially hard in places like California, where many Latinx workers fill essential jobs as farmworkers and meatpackers. “Latino and people of color basically do the scut work that keep the state going, its economy going, but get very little of the resources,” says Dr. David Hayes-Bautista, director of the Center for the Study of Latino Health and Culture at the David Geffen School of Medicine at UCLA. His recent study shows Latinx Californians between the ages of 50 and 64 have died at more than five times the rate of white people of the same age.
Transcript
AMY GOODMAN: This is Democracy Now! The Quarantine Report. I’m Amy Goodman, with Juan González. As states like California see a surge in coronavirus cases and hospitalizations — in fact, California has just surpassed New York in number of cases, though it has a quarter of the deaths of New York — the Latinx community has been especially hard hit.
A new report shows Latinx Californians between the ages of 50 and 64 have died at more than five times the rate of white people of the same age. The report from UCLA, the University of California, Los Angeles, links the trend to the fact that Latinx workers make up the bulk of agricultural workers, who are high-risk essential workers.
In a Frontline PBS documentary called COVID’s Hidden Toll that aired Tuesday night, farmworker Sinthia Hernandez describes how she has both cancer and diabetes, which put her at a higher risk for complications if she were to contract COVID-19, and that the contractor she works for requires her to bring her own mask.
SINTHIA HERNANDEZ: [translated] All us farmworkers are making a big sacrifice out of necessity for hunger, to be able to feed our families and to have a place to live. … Those of us who are working have so much debt and bills to pay that the money sometimes isn’t even enough to buy one mask, because each mask costs $3 or $4 at the store. And it’s disposable.
AMY GOODMAN: Likewise, a report from the Centers for Disease Control found 87% of workers infected on the job at meat processing plants are people of color.
Because of the surge of cases in Los Angeles, it may soon face a second stay-at-home order. This comes as a Los Angeles Apparel factory that employs mostly Latinx workers to produce face masks has been shut down after health inspectors found, quote, “flagrant violations” of infection control orders. More than 300 workers at that one factory tested positive for COVID; four died. The company is run by Dov Charney, former CEO of American Apparel, who was ousted amidst allegations of misusing funds and allowing sexual harassment. Workers said the company failed to clearly inform them when people got sick, or enforce social distancing.
For more, we’re joined by Dr. David Hayes-Bautista, distinguished professor of medicine and director of the Center for the Study of Latino Health and Culture at the David Geffen School of Medicine at UCLA.
It’s great to have you with this, Dr. Hayes-Bautista.
DR. DAVID HAYES-BAUTISTA: It’s great to be here. Great to be here.
AMY GOODMAN: Can you start off by talking about L.A. Apparel, 300 workers found positive, four died, at least, at this point? What do you know about that? And then move on to farmworkers.
DR. DAVID HAYES-BAUTISTA: Well, actually, both of them are related, because these are structural situations. What we’ve noticed is that as soon as the state was locked down the first time, early in March, people were told to work from home, take their children out of school — the children would do their lessons at home — and to leave the house only to buy groceries or the bare necessities. Well, what we discovered, about a month and a half in, is that the essential workers are not only just the nurses and physicians, who, by the way, are trained to go into dangerous situations. They have personal protective equipment. They’re trained to use it. The question was just getting enough to them. But other workers were also as essential in order for the higher-income families to shelter in place, starting with the farmworkers, who, of course, cannot plant strawberries from home. They have to go out on the job. They’re working in large crews. They’re transported on buses. Some of them sleep in barracks.
And as we look at the chain of food — the truck drivers, the packing house workers, the slaughterhouse workers, the grocery store shelf stockers, the grocery store checkout clerks — for Pete’s sake, a checkout clerk would have possibly a couple of hundred people pass within an arm’s length of the checkout stand, and for two months they were not even offered personal protective equipment. Now we’re seeing this in a more industrial, such as in the apparel companies, where, again, for a long time we’ve had costureras working at the bottom, if you will, of the economic chain, paid very little, rarely offered health insurance, rarely offered any education about what’s going on. And now we’re seeing the effects of all of this. So, what we see at a large scale is that Latino and people of color basically do the scut work that keep the state going, its economy going, but get very little of the resources, very little pay, very little health insurance, very little access to care. And this particular pandemic is now exposing these inequities.
JUAN GONZÁLEZ: And, Dr. Hayes-Bautista, in terms of the — given that the Latino population of the United States is significantly younger than either the white population or the African American population, and that this disease especially hits hard in terms of fatality at the elderly, you would expect much lower death rates among Latinos, just because so much of the population is young. Yet you’re seeing — you’re finding, at least especially in the 50-to-65 age range, this enormous disparity in terms of deaths among Latinos. How much of that do you sense is actually as a result of the working conditions that they’re being subjected to, or how much of it is part of the underlying health conditions, whether it’s diabetes or hypertension or other health conditions that many Latinos face?
DR. DAVID HAYES-BAUTISTA: Older populations always have higher death rates for almost anything compared to younger populations. But what’s important here, yes, younger Latinos have a lower death rate than older Latinos; however, when we look at younger Latinos and younger non-Hispanic whites, the Latinos have about four to five times the death rate of whites. So, clearly, something is not working even within that younger population. And again, this has a lot to do with both working and living conditions. We’ve outlined some of them. Let me just go into more detail.
Latinos, even after Obamacare, consistently are twice as likely not to have health insurance. Latinos, for a number of reasons, are faced with a huge doctor shortage, much less being able to find doctors that speak Spanish. And by the way, medical services have been provided in Spanish in California for 251 years. So this is not like this is suddenly a new problem we’ve discovered. This has been a problem ever since 1848.
So, if you remember the early days of the pandemic, Hollywood was able to get access to tests almost immediately. The Lakers got their tests immediately. Those who had access to what’s called boutique medicine got their tests immediately. Well, some of these tests can cost up to $2,000, depending on where you’re getting them. If you don’t have health insurance and you hear that a test can cost hundreds or thousands of dollars, you don’t have access to medical services, or particularly one that you can communicate with, this creates a problem.
And early in the pandemic, the California Department of Health sent out an advisory note — in Spanish, God bless them — and it said, if you have the symptoms, you have a high temperature or you have a dry cough, habla con tu médico, pronto, talk to your doctor now. But what if you don’t have a doctor, you don’t know how to pay a doctor? So, many people were not able to. Thus they continued to work without the personal protective equipment. They were exposed to the coronavirus at much higher rates than people that were able to shelter at home. And, not surprisingly, we started to see the case rates mount, particularly after about six weeks into the coronavirus pandemic. And now it’s progressing to full-blown cases of COVID disease, and, of course, now the mortality. So, that’s the working part.
But then there’s the domestic part. Housing is expensive in California. There’s no question about it. And Latinos occupy those positions, occupations and industries that pay very, very little, don’t provide them health insurance usually. So, in order to live, Latinos tend to have more people per household. And this has been a classic pattern. So you’ll also have more multigenerational households. So, it could be that, yes, the kids are no longer in school, they’re at the house, you have the abuelos, you have the grandparents. But you also tend to have, because of low wages and high costs of housing, more multiple-wage-earner households. That is, the adults, more of them, are going out to work, because they just need to, because it’s hard to live here, which means even though the rest of the household may be sheltering, they are going out and being exposed to coronavirus and bringing it back into the household. So now we’re seeing the result of all of these issues compounded.
The Latino physician shortage is so great in California that the rate at which all the California medical schools graduate Latino physicians, it will take 500 years to make up the shortage for the year 2015. So, I can imagine, here’s Señora Gómez. She’s feeling, “I’ve got a high temperature. I’ve got a dry cough. I need to go see the doctor.” “Oh, come in, Señora Gómez. Oh, you have the symptoms? Take a seat, and the doctor will see you in 500 years.” That’s why we have a problem.
AMY GOODMAN: I want to go to the issue of the meatpackers. For example, the JBS beef plant in Greeley, Colorado, the site of the deadliest workplace COVID-19 outbreak in Colorado, where at least 286 workers tested positive for COVID-19, and six died. The United Food and Commercial Workers put up two billboards in Greeley to remember those who died. This week, JBS agreed to a $1.85-an-hour wage increase, after many of the workers walked off the job earlier this month. UFCW Local 7 responded by calling on JBS to improve safety measures, end what it called its “work while sick culture.” That’s one company in one state. President Trump tried to prevent meatpacking plants from being closed. And you have, throughout states, thousands and thousands and thousands of meatpackers being infected with COVID-19, many dying. Can you talk about this, Dr. Hayes-Bautista?
DR. DAVID HAYES-BAUTISTA: Well, yes, not only meatpacker, any production where you have to have a lot of workers standing in close contact, either with one another or with clients — we can say the same thing with grocery store checkout clerks — without providing them the education, without providing the personal protective equipment, without providing them with health insurance or sufficient wages so that they could buy health insurance, this is all a recipe for a quick spread of the coronavirus. And we’re seeing it play out.
JUAN GONZÁLEZ: And, Doctor, I wanted to ask you — Senate Majority Leader Mitch McConnell, every other word out of his mouth the last few weeks has been that a new congressional bill to address the pandemic must include ending of — removal of liability for employers, in terms of their workers getting sick. Given the reality that OSHA, the federal agency in charge of workplace safety, is virtually nonexistent these days in terms of what it does, do you think that it’s advisable for the Democrats to agree to remove liability from employers if they’re not properly protecting their workers?
DR. DAVID HAYES-BAUTISTA: Well, not only is it not advisable, but, if you remember, the first CARES Act, the COVID relief act, specifically excluded any household in which at least one member was a noncitizen. Now, we’re not talking about undocumented; we’re talking about noncitizens. So, you have a green card holder who’s maybe been here 20, 30 years, has not yet taken that last step to naturalize, the whole household was penalized. They got none of the benefits that everyone was worried that are expiring for everybody else. Latino businesses got very little of the business support.
So here we have a population that gets very little from the sources of support, and yet now even the legal route is being closed off, if in fact their employers are held not liable. And I’m wondering how many of these employers, by the way, even bother to offer health insurance, and usually such employers do not. So, it’s putting this entire population at risk. Nonetheless, and let me hasten to point out, the 60 million Latinos in the United States, two years ago, created the world’s eighth-largest economy — $2.3 trillion. And that’s with all these obstacles, all these barriers, all the name-calling. Just think if we actually invested the way we invested in the rest of the country.
AMY GOODMAN: So, Dr. David Hayes-Bautista, your state, California, has exceeded our state, surpassed New York, in number of COVID infections. Of course, we don’t really know the number of COVID infections anywhere in this country. It’s considered a far underestimate. CDC thinks it’s something like 24 times higher. But can you explain what’s going on, also what’s happening on the border with people who are living on the border? You talked — mentioned undocumented, but what about actually undocumented people in this country having access to healthcare, and the fact that the Trump administration has not made use of $7 billion to $8 billion that were allocated by Congress for testing, for masks, and you have this incredible, severe shortage of all of these things right now, and how that particularly affects the Latinx community?
DR. DAVID HAYES-BAUTISTA: This is a case in point. If you remember the first days of the lockdown across the country, in early March, mid-March, early April, and people ran to the grocery stores, and there was a run on certain products, such as, remember, paper towels and toilet paper, and people were fighting in the aisles over bales of paper towels and toilet paper — in California, 100% of the farm labor workforce is Latino. It’s 100% immigrant, and probably 60 to 80% undocumented. Now, what’s interesting is that, early on, these farmworkers were considered essential employees. In fact, they were given letters that would allow them to actually travel to work without being stopped. And yet, they could also be deported at any moment.
So, between the deportations, between COVID and everything else, if these farmworkers are not allowed at least the opportunity to live, who is going to grow the food? And we thought we were fighting over paper towels and toilet paper? Suppose we’re fighting over the last sack of potatoes in the store. That could happen if this labor force were not here. Yet we criminalize it. We put obstacles for access to care. And then we wonder if we’re going to have a food shortage.
AMY GOODMAN: Language barriers, Dr. David Hayes-Bautista, when it comes to getting information about COVID-19?
DR. DAVID HAYES-BAUTISTA: Medical services have been providing — in fact, we had the first smallpox vaccination campaign in 1803 in California in Spanish. We were part of Spain at the time. Medical services have been provided in California in Spanish for 251 years. We came into the United States as a bilingual state. Spanish was one of the official languages. And yet Latinos are least likely to find a physician who speaks Spanish. The shortage is tremendous.
But it’s not because this is a new issue. This is California. What we have done for 160 years is chosen to turn our back on this population, not allow it access to the investments we were making in other populations either for education or healthcare, then wonder why there’s an issue.
AMY GOODMAN: Dr. David Hayes-Bautista, I want to thank you so much for being with us, distinguished professor of medicine and director of the Center for the Study of Latino Health and Culture at the UCLA medical school. I’m Amy Goodman, with Juan González. Stay safe.












Media Options