
Topics
Guests
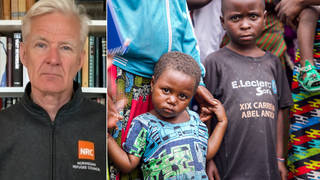
- Peter Hotezco-director of the Center for Vaccine Development at Texas Children’s Hospital and dean of the National School of Tropical Medicine at Baylor College of Medicine.
We look at the state of the pandemic and vaccine rollout in the United States and around the world with Dr. Peter Hotez, co-director of the Center for Vaccine Development at Texas Children’s Hospital and dean of the National School of Tropical Medicine at Baylor College of Medicine. Dr. Hotez is part of a team at Baylor University that is working with a private Indian company to develop a low-cost COVID-19 vaccine. The task of developing a simple vaccine is “daunting,” Dr. Hotez says. “We’re talking about 5 billion doses of vaccine. And the question is: Where do you get 5 billion doses of vaccine?” he says. “We’re trying to come through with something that uses the same old-school technology as the recombinant hepatitis B vaccine that’s been around for four decades.”
Transcript
AMY GOODMAN: This is Democracy Now!, democracynow.org, The Quarantine Report. I’m Amy Goodman. Sign up for our daily news digest email by texting the word “democracynow” — one word, no space — to 66866 today. This is Democracy Now! I’m Amy Goodman, with Nermeen Shaikh.
While India is facing a public health catastrophe from surging COVID-19 cases, the United States reached a milestone Wednesday with the White House reporting it’s reached its goal of administering 200 million vaccine doses within President Biden’s first 100 days. He had originally aimed for 100 million. This comes as the U.S. and other wealthy members of the World Trade Organization continue to fight efforts, led by India, to force Big Pharma to waive patent rights to help address the crisis.
To talk more about the state of the pandemic in the United States and abroad, we’re joined by Dr. Peter Hotez, co-director of the Center for Vaccine Development at Texas Children’s Hospital, dean of the National School of Tropical Medicine at Baylor College of Medicine. He also has a new book out; it’s called Preventing the Next Pandemic: Vaccine Diplomacy in a Time of Anti-science. And he’s part of a team at Baylor which is working with a private Indian company to develop a low-cost COVID vaccine.
Dr. Hotez, welcome back to Democracy Now! We just finished talking —
DR. PETER HOTEZ: Thanks so much for having me.
AMY GOODMAN: It’s great to have you. We just finished talking with Rana Ayyub, The Washington Post opinions editor in India, describing the COVID storm that they are experiencing there. You are coming up with a plan for a low-cost vaccine, working with an Indian company. Can explain what this means? And what are the obstacles to it?
DR. PETER HOTEZ: Yeah, and it’s not only just for India. What we need is a simple, easy-to-use, low-cost, some people call it people’s vaccine for the world, because the task is daunting. We have 1.1 billion people in sub-Saharan Africa, roughly 650 million people in Latin America, at least, you know, close to half a billion or more in low-income areas of Asia. So, you multiply that times two, we’re talking about 5 billion doses of vaccine. And the question is: Where do you get 5 billion doses of vaccine? You know, the mRNA technology is extremely exciting, but it’s new. And whether or not you could ever scale it to that in time for this pandemic is really questionable. So, what else can we come up with?
There’s the adenovirus-vectored vaccines from AstraZeneca and J&J. There’s going to be some issues around vaccine acceptance. Hopefully, that will resolve. But in the meantime, we’re trying to come through with something that uses the same old-school technology as the recombinant hepatitis B vaccine that’s been around for four decades. It’s a microbial fermentation-expressed recombinant protein in yeast, and it looks really good. It’s in Phase — finishing now Phase 2 clinical trials in India, and great protection in nonhuman primates. And now working with Biological E., one of the big private companies, like Serum Institute of India, and they’re based in Hyderabad, they’re now scaling it up to a billion doses. And that’s really exciting. And hopefully it could be released for emergency use authorization by the summer in India.
But then, what about the rest of the world? Biological E. is committed to, I think, providing about 70% of its vaccines to the COVAX sharing facility. But could we get another group to come along and help us with another 4 billion doses? And it would be great if the U.S. government could have a role in that and help reassert some leadership in global health.
NERMEEN SHAIKH: Dr. Hotez, the Biological E. vaccine is reportedly going to cost only $1.50 per dose. Could you talk about why it is — some people have raised the question of why it is that a more accessible, cheaper vaccine, that could easily be transported and stored — why such a vaccine was not invested in earlier, not developed earlier, and whether that could have happened with investment from rich countries.
DR. PETER HOTEZ: Yeah, no, it’s an important — you ask probably the most important question. And we asked it ourselves, because we had been developing coronavirus vaccines for the last 10 years. We work on vaccines for diseases of the poor, that — vaccines that no one else will make. We have a vaccine for schistosomiasis in clinical trials, that’s a huge problem in Africa, for Chagas disease in Latin America. And we adopted a coronavirus vaccine program 10 years ago, because at that time nobody cared about coronavirus vaccines. It was also orphaned. And we figured out how to deliver the spike protein as a low-cost recombinant protein vaccine.
And when we got the COVID-19 sequence in January, our team, which is just co-headed by myself and Maria Elena Bottazzi — we’ve worked together for 20 years — we turned that around really quickly. And then we couldn’t raise money for it, because everybody was so focused on innovation. It was all about innovation, and they wanted mRNA and adenovirus-vectored vaccines. And I said, “That’s great, but what if you can’t scale it, or what if there’s a safety signal? Don’t you want a simple, low-cost vaccine as a backup?” And we just couldn’t get anybody to move. So I wound up raising money privately from philanthropies here in Texas, like the Kleberg Foundation and Tito’s Vodka, of all places, and the JPB Foundation. They came through. I raised about $4 or $5 million. And then we were able to make that — scale up that vaccine and transfer it to Biological E. I often think, though, if I hadn’t had to spend the first few months of the pandemic going out trying to raise money, we could have maybe had something ready to go right now.
So, you know, I think — I can’t complain about the vaccines that we do have. I myself have gotten the Pfizer-BioNTech vaccine, and I’m very grateful for it. But there wasn’t enough attention paid to an unfussy, simple, durable, easy-breezy vaccine for resource-poor countries, which is what we’ve been doing. And hopefully, now we can move this along pretty quickly. Now CEPI, the Coalition for Epidemic Preparedness Innovations, is really helping Biological E. They’re helping support the manufacture, and I’m really grateful for that. And so we’re trying to move as quickly as we can right now.
NERMEEN SHAIKH: Dr. Hotez, could you also talk about some of the other constraints on developing and disseminating vaccines widely? The U.S. has also come under criticism, in addition to patent rights, for maintaining patent rights on these vaccines — it’s also come under criticism for the ban that it’s placed on exporting the raw material for vaccines. Could you talk about what exactly that ban entails and how it’s impacting vaccine efforts around the world?
DR. PETER HOTEZ: Well, I don’t have a lot of details on the ban. One of the things I do know is the Biden administration, through the Quad meetings, I think, was able to relax some of those constraints to support Biological E. and allow some of those raw materials through. So, I’m very happy that they did that.
You know, the patent issue is one that I’m often asked about. And patents are important. One of the things I like to say, though, is, you know, the model of loosening patent restrictions was very much around small molecule drugs during the height of the HIV/AIDS pandemic. And, you know, companies like Cipla, they needed the freedom to be able to make antiretroviral drugs. And patents are important for vaccines, but the most important aspect of vaccines is actually knowing how to make vaccines and knowing how to do it under a quality umbrella with quality control and batch production records, and also having adequate regulatory authorities intact. And that actually tends to be a bigger hurdle than the patents. So, everybody focuses on the patents, based on those earlier models for small molecule drugs, but the forces and the barriers that are around vaccines is a bit different.
What we really need is to train human capital, people, who know how to do vaccines under a quality umbrella in the national regulatory authority, and help with the capacity building. So, the point is, even if you relaxed all the patent restrictions for all the vaccines tomorrow, I’m not certain how quickly that would translate into vaccines for the world for this pandemic. As a long-term issue, definitely it’s important, but right now I think we have to focus on, one, making low-cost, easy-to-use, durable vaccines available to people in resource countries — as I say, 5 billion doses, number one. And number two, let’s start working out that long process of building capacity.
Right now there are no vaccines made on the African continent, or, essentially, no vaccines; not much better in Latin America, a little bit better, but not much; same with the Middle East. And that’s why I served — in the Obama administration, I served as U.S. science envoy to help build up vaccine capacity for Muslim-majority countries in the Middle East and North Africa. It was really exciting to have the opportunity to do that. But we need to figure that out for the rest of the world. We’re still too dependent on the multinational companies for something to filter down.
And, you know, a lot of the innovation right now in the vaccines is not even coming from the big three vaccine companies — Merck, GSK and Sanofi. It’s nontraditional organizations, like Moderna and BioNTech and AstraZeneca, who are not vaccine companies but are accelerating these new technologies. And it’s really important. I think the innovation is really important. I just wish we had balanced the portfolio out a bit more with low-cost vaccines like ours.
AMY GOODMAN: Dr. Ashish Jha, who heads up the Brown School of Public Health, tweeted earlier today, “India is in the throes of a horrendous COVID surge Horrendous They are struggling to get more people vaccinated We are sitting on 35-40 million doses of Astra Zeneca vaccine Americans will never use Can we please give or lend them to India? Like may be now? It’ll help. A lot,” he said. I wanted to get your response to that, Dr. Hotez. Also, how much would it cost for the U.S. to invest? I mean, for God’s sakes, the U.S. is pulling out of Afghanistan. There are many congressmembers who were saying, “Cut the Pentagon budget.” You could take that money saved and pour it into vaccine development, ensuring vaccine equity in the world. So, that’s a two-part question — the AstraZeneca and how much money would it take for the U.S. to give, the way it pours money into weapons development and sales.
DR. PETER HOTEZ: Yeah, so, well, Ashish Jha is a good friend and colleague. He’s a great man. And we talk quite a bit. And I didn’t know he made that statement about the AstraZeneca vaccine, but I think he’s right. There’s no reason to hold onto it. And maybe there are other vaccine supplies that the U.S. can provide for India. And I think they should do that. But we should also remember the scale and scope of this problem right now. India, with a population of — what is it? — 1.2 billion people, they’re going to need 900 million to a billion doses to get — to vaccinate their way out of this. So, in some ways, it’s a drop in the bucket. Yes, they should do it, but, again, the real answer for the coming months is to help accelerate some vaccines like ours.
As far as redirecting budget, you know, who knows how the Office of Management and Budget works in any administration? But, you know, the amount of funding that we would need to scale up production for another 4 billion doses — because, remember, it’s a high-producing yeast strain. It’s low-cost. I think we could do it with a very modest budget. I talk a lot with my friend Jeffrey Sachs, who’s an international development economist, and whenever I tell him about the money we need, he sort of rolls his eyes, and he says, “Oh my god, this is — Peter, this is rounding error, the amount of dollars that you’re talking about. It’s so modest.” And so, if we can just mobilize some of that, I think it would be great.
NERMEEN SHAIKH: Dr. Hotez, very quickly, before we conclude, I’d like to ask you about a recent article you wrote for The BMJ journal, saying that the high death toll from COVID-19 has not arisen from SARS-CoV-2 transmission alone, but also anti-science forces promoting defiance against vaccines. And you talk about the globalization of this anti-vaccine movement. Could you just explain what that is and how that’s happened and how to counter it?
DR. PETER HOTEZ: Yeah, unfortunately, the other hat I wear is a leader in going up against anti-science groups — not by choice, but sort of by default, because in addition to being a vaccine scientist, I am the parent of four adult kids, and my youngest daughter Rachel has autism and intellectual disabilities. And a few years ago I wrote a book called Vaccines Did Not Cause Rachel’s Autism, which made me public enemy number one with the anti-vaccine groups. They call me now the “OG villain,” which I had to look up. It means “original gangster villain.”
And now what was sort of a fringe element — and you’re seeing this play out nightly now on conservative news outlets — they’re now mainstream among the conservative parties — in the U.S., our Republican Party. And that’s really scary. And then you’ve got the Russian government launching an entire program of what’s being called weaponized health communications, trying to discredit Western vaccines in favor of Sputnik V, or Sputnik 5. And now this is globalized, and you’re seeing the same kind of far-right, U.S. QAnon focus around the anti-vaccine movement now appearing in protests in Western European capitals.
So, I call this an anti-science empire. I tend to be a bit out there on this, in the sense that there’s not, by any means, consensus in the global community that it’s reached that stage. But, you know, I’m of the opinion that when so many lives were lost in the United States not only because of COVID-19, but of deliberate defiance to things like masks and social distancing — and now we have four independent news polls all pointing to the most vaccine-hesitant group in the United States are what are being called Republicans. Some polls call it white Republicans. And that is the reality. There’s been a politicization of the anti-science, anti-vaccine movement.
And we have to figure out a way to dial it back, bring it back. I’m trying to reach out to conservative groups whenever I can, just because we’ve let this thing get out of hand. Neither the U.S. government or the United Nations agencies has really wanted to confront this and really call it out and, you know, express concern to the Putin government and confront them on it, express concern in the U.S. about how we’ve allowed this to globalize. But we have to figure out a way to dial this back.
AMY GOODMAN: Dr. Peter Hotez, we want to thank you for being with us, co-director of the Center for Vaccine Development at Texas Children’s Hospital. Congratulations on your book, Preventing the Next Pandemic: Vaccine Diplomacy in a Time of Anti-science.
When we come back, it’s Earth Day. We’ll hear about The Red Deal. Stay with us.











Media Options