
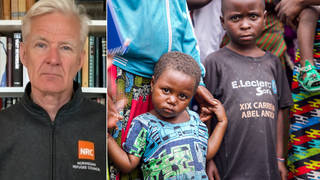
Guests
- Achal Prabhalacoordinator of the AccessIBSA project, which campaigns for access to medicines in India, Brazil and South Africa.
- Leena MenghaneyIndian lawyer who has worked for two decades on pharmaceutical law and policy and heads Médecins Sans Frontières’s access campaign in India.
We look at the urgent push to ensure equal access to COVID-19 vaccines for all nations, rich and poor, and growing calls for Big Pharma to waive their patent rights, as COVID-19 cases soar in India and the Modi government has suspended exports of coronavirus vaccines to many of the world’s poorest countries that depend on AstraZeneca vaccines it produces. “These are not India’s vaccines,” says Achal Prabhala, coordinator of the AccessIBSA project, which campaigns for equitable access to medicines. “The number of vaccine doses that have gone out to a third of humanity — 91 poor countries — is 18 million doses, or just enough to cover about 1% of the populations of these countries if they’ve even got vaccines, which some have not,” Prabhala notes. Leena Menghaney, an Indian lawyer who heads Médecins Sans Frontières’s access campaign in India, links the supply shortage to Oxford University’s decision to sign an exclusive deal with the Serum Institute in India rather than contracting several manufacturers to produce the vaccine. “The monopoly is going to cost us,” Menghaney says.
Transcript
AMY GOODMAN: We begin today’s show with the urgent push to ensure equal access to COVID-19 vaccines for all nations, rich and poor, and growing calls for Big Pharma to waive their patent rights. As Christians around the world marked Easter Sunday, Italy moved up midnight Masses to meet a 10 p.m. curfew amidst a spike in COVID cases. And Pope Francis used his Easter Mass address at St. Peter’s Basilica in the Vatican to warn against vaccine nationalism.
POPE FRANCIS: [translated] In the spirit of an internationalism of vaccines, I urge the entire international community to a common commitment to overcome the delays in their distribution and to promote their distribution especially in the poorest countries.
AMY GOODMAN: According to Oxfam, rich countries, with just 13% of the world’s population, have bought up more than 60% of vaccines even before their production. This comes as COVAX, the United Nations initiative to bring mass vaccination to poorer countries, has placed orders for more than 2 billion shots, but most of them won’t come until the second half of this year.
Meanwhile, deliveries from the world’s biggest coronavirus vaccine manufacturer in India have been delayed as COVID-19 cases soar to record highs in India and the Modi government has suspended vaccine exports. With more than 12.6 million confirmed coronavirus cases, India has the world’s third-highest caseload, after the United States and Brazil.
On Sunday, the head of the public-private GAVI Alliance, which works to provide vaccines to the developing world and is backed by the United Nations and the Gates Foundation, addressed the delay during an interview on CBS’s Face the Nation. This is Seth Berkley.
DR. SETH BERKLEY: So, India is, by volume, the largest supplier of vaccines for the developing world. And because of the new wave of outbreaks in India right now, the Indian government has stepped up their vaccination programs. And that has meant that they’ve required more doses, which means that they’ve made less doses available for the rest of the world. We had expected, in March and April, about 90 million doses, and we suspect we’ll get much, much less than that. And that is a problem.
But we’re in a race, because we also see wealthy countries beginning to cover much of their population, and our hope is that they will begin to make their vaccines available to the rest of the world, including ones that they may not use. For example, the U.S. not only has Moderna, Pfizer and J&J, but they also have vaccines from Novavax and, of course, from AstraZeneca. Those could be made available, and they would make a big difference in terms of the supply for the world.
AMY GOODMAN: Well, our next guests write about this in a new piece for The Guardian headlined “The world’s poorest countries are at India’s mercy for vaccines. It’s unsustainable.” In it, they note that as the U.K. saw a delay in doses from India, quote, “a far more chilling reality was unfolding: about a third of all humanity, living in the poorest countries, found out that they will get almost no coronavirus vaccines in the near future because of India’s urgent need to vaccinate its own massive population.
For more, we go to India, where we’re joined in Bangalore by Achal Prabhala. He is the coordinator of the AccessIBSA project, which campaigns for access to medicines in India, Brazil and South Africa. And in Delhi, Leena Menghaney is with us, an Indian lawyer who has worked for two decades on pharmaceutical law and policy. She is head of the Médecins Sans Frontières — that’s Doctors Without Borders — access campaign in India.
We welcome you both to Democracy Now! Achal Prabhala, it’s great to have you back. You co-authored this piece. Elaborate further on what is taking place, this as we hear Pope Francis’s address demanding the wealthy countries ensure that the world gets these vaccines, especially the poorest countries.
ACHAL PRABHALA: Thank you.
What we’re seeing now is a failure that was foretold over a year ago, when vaccine manufacturing and vaccine research just began. What’s happening today is a set of cumulative failures over the last year, many of which were predicted, many of which could have been avoided.
Of the vaccines available in the world, there are vaccines from Pfizer and Moderna which are simply not available outside rich countries. AstraZeneca is one of the few companies that has made its vaccine a little more available, primarily by signing an agreement with the largest vaccine manufacturer in the world, who happens to be located in India. Now, the problem is that what they signed over were the rights to supply vaccines to 92 poor countries around the world, including India, essentially to one vaccine manufacturer, with very, very few backups. What that’s meant is that you have these 92 countries that are dependent upon one company that operates on Indian soil.
Now, by its share of population, India should get about 35% of these vaccines. What’s happening instead is that the Indian government is acquiring far more of those vaccines than 35%. At this moment and for the next couple of months, it’s going to be closer to 100%. The problem with this is that these are not India’s vaccines. These vaccines were always meant, contractually, for about half of humanity, including India. Now, they’re not getting there. Seth Berkley, the head of the COVAX initiative, which promised to provide a pipeline of vaccines to these poor countries last year, has said that he hoped to have 100 million doses out. The reality is so much worse, because what he has out are 28 million vaccines, 10 million of which went right back to India. So the number of vaccine doses that have gone out to a third of humanity — 91 poor countries — is 18 million doses, or just enough to cover about 1% of the populations of these countries if they’ve even got vaccines, which some have not.
AMY GOODMAN: [inaudible] Leena Menghaney about the consequence of the contract between Oxford and AstraZeneca with the Serum Institute in India, just to explain for people to understand what is taking place and the role of these large pharmaceutical companies.
LEENA MENGHANEY: Yeah. I’ve worked in pharmaceuticals and biopharmaceuticals for 20 years. And the rule is, you have to have at least three suppliers. If you look at India itself, it has many manufacturing sites and many manufacturers. The decision to go and have an exclusive deal with Serum Institute is going to cost lives, because that’s exactly where it all started, with Oxford granting exclusive rights to AstraZeneca, and AstraZeneca choosing to tie up with one single manufacturer.
We all know that India is the pharmacy of the developing world. They could produce more, and they should have transferred technology and the rights to produce these vaccines to more than one company. The monopoly is going to cost us. We need to have scaled up not with just Serum Institute, but a large number of other manufacturers in India.
So, now India is in this difficult position where it has to vaccinate its own people at a faster and faster pace to beat the epidemic, and then, at the same time, actually ensure that these vaccines go to the developing world. We’re at a very difficult point in India’s, you know, policymakers’ — I wouldn’t want to be in their shoes today.
AMY GOODMAN: Achal, you write in the piece with Leena, “The billions of AstraZeneca doses being produced by the Serum Institute in India are not for rich countries — and, in fact, not even for India alone: they are for all 92 of the poorest countries in the world. … [T]he bulk of India’s vaccination goals will be met by just one supplier, which faces the impossible choice of either letting down the other 91 countries depending on it, or offending its own government.” Can you talk more about this and the gross vaccine inequities we’re seeing across the globe?
ACHAL PRABHALA: Absolutely. One of the interesting things about this is how it begins. Oxford University has a research laboratory called the Jenner Institute, which shows early promise on research for a coronavirus vaccine. This is at exactly this time last year, in about March. They suggest, in public statements, that they would like to have as many manufacturers around the world make the vaccine. It’s not necessarily nonprofit or technically open source, but they have this idea of a world in which anyone can make their vaccine. The Gates Foundation steps in, advises the Jenner Institute to go with a pharmaceutical company. One month later, they sign an exclusive contract with AstraZeneca, a U.K.-based multinational pharmaceutical corporation. AstraZeneca then licenses a large number of doses to the Serum Institute in India; they license a firm in South Korea — both of which are now producing vaccines. But what they do is that they transfer one concentration of monopoly power to another manufacturer with another kind of monopoly power, the monopoly power to supply half the world’s population, including India, with a number of vaccine doses that is simply not enough.
One of the funny things about this is that it’s as though everybody involved, from the Gates Foundation to AstraZeneca and, unfortunately, including the government of India — it’s as though they suddenly realized how many people live in India. Our population is not a secret. We have 1.3 billion people. We’ve always known that these people would require vaccines. And yet it seems to have taken the government of India until about two months ago to discover that we would have to ramp up our vaccination program, at which point they decided, through this result of colossal bad planning and cumulatively bad decisions, to essentially usurp vaccines that were meant for other poor countries, who do not have the kind of vaccine manufacturing capacity India does. And because they’re being made within Indian sovereign territory, they are actually able to do that, to the detriment of countries like Ghana or Nigeria, who have received enough doses to inoculate 1% of their population, will now have to wait at least until July this year, but possibly much longer, because India’s vaccination needs, as well, will continue to be met by this one company, where all the vaccines — where all the vaccine doses are concentrated for all of these countries for the next several months.
AMY GOODMAN: Leena, can you talk about the need, the — what you’re calling for, with the People’s Vaccine initiative around the world, as well, calling for this, as well as countries like India and South Africa, calling for pharmaceutical — the WTO and the U.S. to support the waiving of patents by pharmaceutical companies?
LEENA MENGHANEY: Yeah. So, this proposal is quite interesting. It shifts power from pharmaceutical corporations to government. And what it really says is that we learn from experience. In HIV/AIDS, we had to overcome patent barriers country by country, drug by drug. And instead, what they have proposed is that we waive our intellectual property automatically in one go, you know, saving a lot of time along the way in producing not just vaccines, but medicines and other medical products.
So, in a nutshell, what India and South Africa proposed and asked the world to support them on was that we don’t have to do this the hard way. We don’t have to lose lives like we did in the HIV/AIDS epidemic. We don’t have to overcome patents country by country. And what we do is an automatic waiving of intellectual property monopolies. And that actually could result in fastening of, you know, production in many new regions and countries who are investing in sort of coming into making pharmaceuticals and vaccines.
AMY GOODMAN: And, Achal Prabhala, can you also elaborate on this? There’s been a big push. We just spoke with the former foreign secretary of Brazil. And, of course, COVID is just exploding there. And he also expressed grave disappointment in the Biden administration for not supporting the call at the WTO to waive the intellectual rights of these corporations during the pandemic.
ACHAL PRABHALA: There’s no choice. They must. If they wish to have a solution that works not only for the rest of the world, poor countries, but also for them, eventually, in their own selfish interests, they must find a way to waive or suspend pharmaceutical monopolies in the pandemic.
Interestingly, one of the things that’s happening at the World Trade Organization is that this AstraZeneca access agreement, that we analyzed, which has turned out to be quite catastrophic, is being held up as the example. We’re criticizing AstraZeneca, but that’s because they’ve actually done something to make access available. Companies like Pfizer and Moderna, and even Johnson & Johnson to a certain extent, have done nothing.
Now, AstraZeneca’s licensing agreement, however much it’s a step up from what Pfizer and Moderna have done, is, in fact, a failure. It’s not working out. It’s inadequate. It needed to have been bigger and better and taken into account the real needs of the real people who live in this world. So, the idea that you can leave it up to pharmaceutical companies to occasionally license their products and to slightly distribute the extreme concentration of power that they have, which is a proposal being actively discussed at the WTO, is foolish. And I hope that the example of how the AstraZeneca agreement has worked out will serve as caution for the fact that nothing other than a dramatic step to suspend pharmaceutical monopolies all over the world will get us out of this pandemic.
AMY GOODMAN: Achal Prabhala, you talk about Oxford University’s original motivations for developing the vaccine, and you talk about motives being thwarted by the Gates Foundation. How?
ACHAL PRABHALA: Oxford University had this idea that since we were in a pandemic that created this global emergency, they must do something that would step out of the norms of the kind of pharmaceutical research they do. What they wanted to have, very clearly expressed by the lead researchers, by Adrian Hill and Sarah Gilbert at that time, was to be able to license as many manufacturers as possible around the world. I don’t think they ever intended to lose money, but they didn’t intend to turn it into the kind of pharmaceutical juggernaut that coronavirus vaccines have become. This was very clearly expressed.
But very quickly, on the advice of the Gates Foundation and a few other parties — the U.K. government was involved — the contract completely changed, and the system of licensing this vaccine was dramatically reversed. They signed an exclusive contract with AstraZeneca, that then further went out and created a handful of these access licenses, of which it’s only truly one that functions and serves for half the world’s population.
It’s a mistake of tragic proportions that I’m not sure every party involved understands. I believe they were working with the best intentions, but they were working without an understanding of the last 20 years of human history. It’s a mistake that should definitely not be repeated, certainly not be held up as a solution, and it’s something that we need to reverse and correct at this moment.
AMY GOODMAN: And finally, you mentioned that while you are very critical of AstraZeneca, that Moderna and Pfizer’s contracts are worse. Explain.
ACHAL PRABHALA: Pfizer and Moderna are running on this model where they believe supplying literally between 15 and 20% of the world, which is the cumulative population of everyone who lives in rich countries, is sufficient. They will not do a thing more than that. Eighty percent of the world or 85% of the world is being left out to dry.
The idea is that they are going to places where they have high-paying customers, usually in the form of governments, from whom they have these huge preorders. Moderna posted revenue of $18 billion this year, so they’re doing well out of this strategy. And their idea is to limit the production of vaccines to the people who can afford them, to safeguard their relatively new technology of a messenger RNA platform that they’ve deployed in this vaccine, to protect that platform against future exploitation, against future commercial use. To the extent that it is democratized and there are more people who can manufacture this around the world, even in the pandemic, I think it threatens their ability to exploit the platform in the future. So the idea is to hold this close, to serve in the pandemic those who can pay, and pay no heed and no mind to anybody who lives outside this tiny handful of countries that they’re currently serving and doing very well for them.
AMY GOODMAN: And as we know from the pandemic, what it has taught us, if nothing else, if one person is sick somewhere, everyone has the potential to be sick. I want to thank you, Achal Prabhala, coordinator of the AccessIBSA object, which stands for India, Brazil, South Africa, and Leena Menghaney, heads up Médecins Sans Frontières, Doctors Without Borders, access campaign in India. We’ll link to your op-ed in The Guardian, “The world’s poorest countries are at India’s mercy for vaccines. It’s unsustainable.”
When we come back, we go to Ethiopia, where rape is being used as a weapon of war in its military offensive in the Tigray region. Stay with us.












Media Options