
Topics
Guests
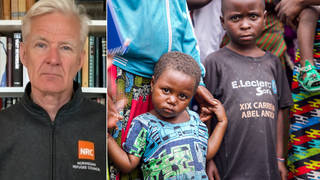
- Abraar Karaninternal medicine doctor and infectious disease fellow at Stanford University School of Medicine.
After months of decline in COVID-19 cases in the United States due in part to widely available vaccines, the number of new cases per day is on the rise again. Pfizer representatives met with U.S. regulators and vaccine experts to seek emergency use authorization for a second booster dose of its vaccine, as health experts are continuing to highlight the growing gap in administered vaccinations between rich and low-income countries. “In the United States, we have access to multiple vaccines,” says Dr. Abraar Karan, an internal medicine doctor and infectious disease fellow at Stanford University School of Medicine. “Many countries have not seen any vaccine at all.” He also says it’s too early to say whether a third vaccine dose is necessary, as Pfizer has insisted. “I hope the science is what guides this, not the financial aspects,” he says.
Transcript
AMY GOODMAN: This is Democracy Now! I’m Amy Goodman, with Juan González.
After months of decline in COVID cases in the United States, due in part to widely available vaccines, the number of new cases per day is on the rise. This comes as Pfizer officials met with U.S. regulators and vaccine experts Monday seeking emergency use authorization for a third shot, a booster. Most public health experts say a third shot of Pfizer’s mRNA vaccine is not necessary for most adults.
Meanwhile, in Geneva, Switzerland, the head of the World Health Organization slammed the growing vaccine gap between rich and poor countries. This is Dr. Tedros Adhanom Ghebreyesus.
TEDROS ADHANOM GHEBREYESUS: Some countries and regions are actually ordering millions of booster doses before other countries have had supplies to vaccinate their health workers and most vulnerable. … We’re making conscious choices right now not to protect those most in need.
AMY GOODMAN: Meanwhile, the U.S. Food and Drug Administration has added a new warning to Johnson & Johnson’s single-dose COVID-19 vaccine. The FDA reports about a hundred cases of the rare autoimmune disorder Guillain-Barré among 12.8 million J&J vaccine recipients in the U.S. The cases were mostly in men aged 50 and older, with one death reported. The FDA said, in a statement, the benefits of the vaccine still clearly outweigh the risks.
For more, we’re joined in Palo Alto, California, by Dr. Abraar Karan. He’s a fellow at Stanford University in the Division of Infectious Diseases and Geographic Medicine.
Doctor, welcome back to Democracy Now! It’s great to have you with us. Why don’t we start off with you explaining this latest development with Johnson & Johnson, and then move on to what Pfizer is asking for, the third booster [sic], and the vaccine gap in the world?
DR. ABRAAR KARAN: Definitely. Thanks so much for having me, Amy.
So, in terms of the Johnson & Johnson vaccine, as we had noted earlier, when there was a signal for the brain clots in younger women, now there is a signal — an association, but we can’t say it’s a causation — of Guillain-Barré syndrome, which is an autoimmune condition. It’s a neurologic syndrome in which the immune system attacks the nerves and can give you paralysis, can take weeks, or even years, in some people, to fully resolve. It’s a serious condition. We usually actually see this after different respiratory viral infections. You can see it after COVID. Most cases are actually after Campylobacter infections. Forty percent or so are thought to be caused from this in the United States. I think, as you mentioned, there’s about 3,000 to 6,000 cases per year.
And so, what you note here, though, is that there may be a slightly higher incidence in men above age 50 who have taken the J&J vaccine. So, what that means is, essentially, the CDC’s Committee on Immunization Practices will have to review this and see if, in fact, there is enough data to link the two. And if so, they may give recommendations for specific groups, such as men in that age group. Perhaps if they can get a mRNA vaccine, they made recommend that.
But with that being said, even with COVID, you can see — and you often do see — many neurologic sequelae. And so, again, the risk is always weighing against the benefit, the risk of getting COVID, getting other symptoms from it, versus the benefit of getting the vaccine. And, you know, in the United States, we have access to multiple vaccines, including the mRNA vaccines, where they have not seen this signal. And so, we have options here, whereas in many other parts of the world, unfortunately, as Dr. Ghebreyesus mentioned, there isn’t that option. Many countries have not seen any vaccine at all.
And so, that actually brings me to the next point, which is the Pfizer vaccine and the need for a booster shot. So, essentially, what they’re saying is that there’s data that Pfizer has, that they’ve reviewed with top health officials in the U.S., suggesting that patients who are immunocompromised, such as patients who have recently received transplants or immunosuppressive therapies, may have a higher risk of getting COVID even after they’ve been fully vaccinated. Now, I haven’t seen all of that data. It hasn’t been fully publicly released. And so, that will really depend on what we are seeing. Now, remember, that’s against the background of the Delta variant, more transmissible variant, and variants that are more virulent, as well, that can cause more disease, and also the fact that, you know, for many people now, it’s been several months since they received their vaccines. I received mine back in January. So there’s a lot of things at play here, and we need more data before we make any final decisions.
JUAN GONZÁLEZ: And, Doctor, we’ve heard a lot about the Delta variant. Could you talk about the Lambda variant, what we know about it at this time?
DR. ABRAAR KARAN: Well, you know, with all of these variants, essentially, the main questions are: How transmissible is the variant? Is it able to outcompete other variants that are present? And what specific mutations are there in the receptor-binding domain, which is essentially the domain and different proteins around there through which the virus binds and enters cells? You know, this — we really look to our virology colleagues to parse through some of that data. I work more on the epidemiologic side. And so, there, you essentially have to see what percent of cases are being caused by different variants, how are they competing against one another in different populations. And so, you know, at least speaking to Delta variant, we know that a few months ago it only comprised about 3% of cases in the U.S. Now it’s, you know, closer to 60% of cases. And that has been rising pretty quickly. I don’t have the data right on hand for Lambda variant.
AMY GOODMAN: And last few seconds, on this issue of Pfizer pushing for the third, the booster, do you think there is a financial incentive here for them?
DR. ABRAAR KARAN: Well, you know, you always have to wonder with pharmaceutical companies, especially given that it is an industry that is, you know, very profitable, and we’ve seen a lot of vaccine inequity globally. I work as a global health physician, and so I always scrutinize some of these decisions. With that being said, I want to look to the actual primary data and analyze that for myself. So, when we do have access to that data, we hope to see it, and, you know, there’s a lot of us looking at this very closely. And so, I hope the science is what guides this, not the financial aspects.
AMY GOODMAN: We want to thank you so much for being with us, Dr. Abraar Karan, fellow at Stanford University in the Division of Infectious Diseases and Geographic Medicine.
That does it for our show. Democracy Now! is produced with Renée Feltz, Mike Burke, Deena Guzder, Messiah Rhodes, Nermeen Shaikh, María Taracena, Tami Woronoff, Charina Nadura, Sam Alcoff, Tey-Marie Astudillo, John Hamilton, Robby Karran, Hany Massoud and Adriano Contreras. Our general manager is Julie Crosby. Special thanks to Becca Staley, Miriam Barnard, Paul Powell, Mike DiFilippo, Miguel Nogueira. I’m Amy Goodman, with Juan González.











Media Options