
Guests
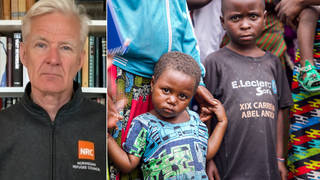
- Nick MaynardBritish surgeon who led an emergency medical team at Gaza’s Al-Aqsa Hospital, former director for cancer services at Oxford University.
We speak with British surgeon Dr. Nick Maynard, who recently led an emergency medical team at Gaza’s Al-Aqsa Hospital, about Israel’s ongoing attacks on healthcare infrastructure and the worsening humanitarian crisis in the besieged territory, where Israel’s brutal assault has killed about 32,000 Palestinians since October 7. Maynard is part of a group of international doctors with experience in Gaza who met with officials at the United Nations and in Washington, D.C., this week to express alarm over civilian suffering. Medical workers in Gaza are “working under extremely challenging conditions with a huge lack of resources and working in a healthcare system that is being systematically dismantled by the attacks on it,” he tells Democracy Now! “It’s very, very clear to all of us who have been on the ground in Gaza that the only way to try and stop this humanitarian catastrophe is for an immediate ceasefire.”
Transcript
NERMEEN SHAIKH: Israel’s assault on Al-Shifa, the largest hospital in Gaza, has entered a fourth day. Al Jazeera is reporting Israel has blown up the entire specialist surgery center at the hospital, where thousands of Palestinians had sought refuge and medical care. Israel has now ordered everyone to evacuate as it threatens to blow up the entire medical complex. The World Health Organization says it has documented 410 attacks on healthcare facilities since Israel began its assault on October 7th.
We begin today’s show looking at the collapse of Gaza’s medical system. A group of international doctors who recently spent time in Gaza traveled to the United Nations and Washington this week to express alarm over the humanitarian crisis. This is Amber Alayyan with Médecins Sans Frontières, or Doctors Without Borders, speaking at the United Nations on Tuesday.
DR. AMBER ALAYYAN: Two populations are particularly vulnerable. Pregnant and lactating women, who were already facing iron deficiency anemia before the war, which puts them at risk for hemorrhage during birth, with the war, it puts them in a state of undernourishment or malnutrition, potentially malnutrition, which means that they can’t breastfeed their children properly. The milk doesn’t necessarily come in, and it’s definitely not enough. And the other population is children under 2 years, which is the breastfeeding age.
There’s not enough space for us to work closely with the mothers to help them start lactating again. We can’t even access them. And to be able to do that, you have to have day-to-day activities with those women, and that is not something that’s possible for us right now. Those children need to be breastfed. If they can’t be breastfed, they need formula. To have formula, you need clean water. None of these things are possible. What we’re talking about is women who are squeezing fruits, dates into handkerchiefs, into tissues, and feeding — drip-feeding their children with some sort of sugary substance to nourish them.
NERMEEN SHAIKH: That was Dr. Amber Alayyan of Médecins Sans Frontières. Dr. Zaher Sahloul, the president of MedGlobal, also spoke at the United Nations on Tuesday.
DR. ZAHER SAHLOUL: This is Hiyam Abu Khader. She’s 7 years old. She is one of the victims of the war in Gaza. A bomb hit her family home, so her father and brother were killed. And her mother also was injured, and she had burns. And she sustained third-degree burns on 40% of her body. She was treated by one of our volunteers, Dr. Vanita Gupta, who is a critical care specialist from New York, in the European Hospital in Deir al-Balah. And Dr. Gupta took some videos of her, and you can see her face in the videos, and also in this picture. And if you want to define post-traumatic stress disorder, this is what post-traumatic stress disorder looks like in the face of a child who’s 7 years old. She was supposed to be evacuated to Egypt, and she waited for weeks before she was eventually evacuated, and she died two days after evacuation, because it was too late.
AMY GOODMAN: And professor Nick Maynard also spoke, a surgeon who led an emergency medical team in central Gaza at Al-Aqsa Hospital in December and January, former director for cancer services at Oxford University.
DR. NICK MAYNARD: I saw things at Al-Aqsa Hospital which I still wake up at night thinking about — appalling injuries in particularly women and children, the most devastating burns in small children. One child that I’ll never forget had burns so bad, you could see her facial bones. We knew there was no chance of her surviving that, but there was no morphine to give her. So, not only was she inevitably going to die, but she would die in agony.
AMY GOODMAN: And professor Nick Maynard joins us now, a surgeon who led the emergency medical team in central Gaza at Al-Aqsa Hospital in December and January, again, former director for cancer services at Oxford University.
Dr. Maynard, thanks so much for joining us from Washington. You were here in New York yesterday addressing members of the United Nations. Talk further about what you found, and talk about how it compares. You’ve been going to Gaza for, oh, the last 15 years.
DR. NICK MAYNARD: Yeah. Thank you very much for asking me on this morning.
As you said, I’ve been going to Gaza since 2010 and have worked extensively in various hospitals in Gaza. And each trip, it’s always very challenging. But there are circumstances we get used to. It’s what I describe as “normal Gaza” for people who have been there. It’s, of course, not normal by anyone else’s standards, because there’s always a lack of resources. You’re always wondering whether things are going to be running out. When you’re operating in the operating theaters, you always have to work with the equipment you’re given. It’s never quite enough. But, of course, you manage that very well.
What we’ve seen since October the 7th in the visits we’ve had to Gaza have been inestimably worse than that, and working under extremely challenging conditions with a huge lack of resources and working in a healthcare system which is being systematically dismantled by the attacks on it.
NERMEEN SHAIKH: And, Dr. Maynard, as you know, since you’ve returned, the situation has gotten immeasurably worse. If you could comment on the latest news about the sustained attacks on Al-Shifa Hospital? You said earlier, after your trip in January to Gaza, accusing Israeli forces of, quote, “appalling atrocities” as they systematically targeted hospitals and healthcare infrastructure in Gaza. So, if you could elaborate on that and what you hear of what’s been happening in the last few months since you left?
DR. NICK MAYNARD: Yes, absolutely. I mean, I’ve witnessed myself attacks on hospitals. When I was in Al-Aqsa Hospital, we were forced to withdraw two days early, because there was a missile attack on the intensive care unit.
What’s happening at Shifa Hospital now is really a replica of what happened in the earlier part of this war when Shifa Hospital was attacked and almost completely disabled. I have been in contact with a close friend who is a senior surgeon at Shifa to hear what’s happening in the last 48 to 72 hours. And the same thing is happening again. The hospital, which had been largely disabled, had been beginning to function again in recent weeks, and still at a much lower level than it had originally been capable of, but nevertheless the staff there heroically treating their patients with limited resources. But again, they’ve been forced to leave. I’ve heard horrific testimonies of the medical staff being stripped naked, some of them being abducted again. And we are seeing really the horrors that we witnessed several weeks ago. And Shifa Hospital, of course, being the largest hospital in Gaza, the major trauma center, now again will be almost completely disabled, and there will be no healthcare services for those patients in Gaza City and north Gaza.
NERMEEN SHAIKH: Well, as you know, Dr. Maynard, the U.N. has said that none of Gaza’s 36 hospitals are at this point fully functional. You described your own time working in Al-Aqsa in January as perhaps the worst experience in your medical career. We heard you speak a little bit about this earlier, but if you could describe the conditions under which you worked there and what you saw, the patients that you were seeing, you know, their injuries? If you could just talk about that?
DR. NICK MAYNARD: Yes. We hear a lot about fully functioning and partly functioning hospitals in Gaza. I would argue there have been no fully functioning hospitals at all since October the 7th. The quality of care that I’ve witnessed in over the 15 years I’ve been going has been quite fantastic, some extremely talented doctors and nurses and other healthcare workers providing a remarkably high level of healthcare provision despite the really challenging lack of resources. But even though there is talk about fully functioning and partly functioning, I would argue that even Al-Aqsa Hospital, when I was working there, the Nasser Medical Complex, the European Hospital, before they were attacked by the Israeli forces, they weren’t fully functioning. They could barely cope — well, they couldn’t cope with the numbers of severe traumas coming in. And really, since October the 7th, no hospital facility has been managing to treat patients without trauma, all the communicable and noncommunicable diseases. So, I don’t think any hospital is functioning properly at all, and won’t do so until there is a cessation of the military activity.
When I was in al-Aqsa Hospital, we had very limited resources. I was operating most days — I’m a surgeon, so I was operating on major blast injuries to the abdomen and to the chest. I saw appalling injuries, mostly in women and children, but also in some men, as well. And we operated under very challenging circumstances. Some days there were no sterile drapes to use to cover patients, so we had to make our own out of gowns. Some days there was no running water, so we couldn’t scrub up properly. We had to try and sterilize our hands with alcoholic gel. The equipment we had to use in the operating theater was very limited, very limited numbers of sutures and needles to use, and very few instrument sometimes.
AMY GOODMAN: Dr. Maynard —
DR. NICK MAYNARD: So, really — yeah.
AMY GOODMAN: Can you tell us more about that little girl that you described at the news conference you held at the United Nations with the other doctors?
DR. NICK MAYNARD: Yes. This was a little girl who was managed by one of my close colleagues from Oxford, Dr. Debbie Harrington. It was a little girl with severe burns, whose burns were so severe that you could see her facial bones through the burns. There was no prospect of her surviving these burns, and we knew she was going to die. But there was no morphine available in the emergency room that day. And that was a frequent occurrence during our stay there. So, we knew she was going to die, but she had to die in agony. There was no way of relieving her pain.
And what made it even worse, if it could be worse than that, was the fact that there was nowhere for her to die in privacy. She was lying on the floor of the emergency room at Al-Aqsa Hospital. There was nowhere else for her to go. So she died in public and in agony.
And we witnessed many other examples like that, and I could spend a lot of time talking about the horrible things we saw, people dying without dignity, without pain relief. And I bore witness to things I would never, ever have expected to have seen in any healthcare setting.
AMY GOODMAN: Dr. Maynard, can you talk about the condition of the doctors? A few months ago, we interviewed Dr. Hammam Alloh, who was at Al-Shifa, and he would later die in a bombing. I had asked him why doesn’t he leave, and he said, “Do you think that’s why I went to medical school? To desert my patients?” But can you talk about right now the number of doctors who have been arrested, who have died, who are hungry as they try to work?
DR. NICK MAYNARD: Yes. I’ve been profoundly humbled by the healthcare workers that I’ve met in Gaza, some of whom I’ve known for many years, some of whom I met during my stay at Al-Aqsa Hospital. They’ve been working nonstop under the most appalling conditions since October the 7th. I go out to Gaza with Medical Aid for Palestinians. They have some heroic staff on the ground there who, again, are working under appalling circumstances. One of them who lives in northern Gaza couldn’t move south because of his elderly parents. They’ve been living on birdseed. They’ve run out of animal feed now, so they’re now eating birdseed. I’ve met doctors and nurses who have been physically and mentally broken by what they’re going through, but still carry on working, refusing to leave their patients, because that is what their job is. None of these people have been paid at all since October the 7th, and, indeed, many of them hadn’t been paid for many months up 'til then. But they stay with their patients, because that is their job, that is their duty. And they will not leave, despite the full knowledge that they may die as a result of that. So, I am truly humbled by the people I've met there, both doctors and nurses and some very close friends I’ve made in Medical Aid for Palestinians who work on the ground there.
NERMEEN SHAIKH: Well, Dr. Maynard, I want to ask about another — a related issue, which is, you said that most of the people you treated were women and children. Now, of course, Gaza is on the brink of famine, and at least 27 children have already died of malnutrition as Israel continues to block humanitarian aid supplies. If you could talk about whether you already saw signs in January of the effects of insufficient food on the children that you were treating?
DR. NICK MAYNARD: Yeah. You played earlier the very eloquent description by Amber about the problems with malnutrition in women and children. We saw this when we were there in December and January. We saw at Al-Aqsa Hospital the pediatricians who we knew there were seeing two or three cases a week in December of kwashiorkor. This is the most severe form of protein-deficient malnutrition. And you may remember pictures of the various famines over the years we’ve seen in Africa with potbellied children. And this is the most severe form of malnutrition. And the pediatricians were seeing this in Al-Aqsa back in December.
We saw evidence of — very clear evidence of malnutrition in some of our surgical patients in Al-Aqsa Hospital. Virtually all the patients get severe infective complications of their injuries in their surgery because of the conditions, the overcrowding, the lack of antiobiotics, the lack of sterile procedures. And, of course, when people get these infections, when they develop sepsis, that rapidly accelerates the malnutrition. And these people who were already on the brink of malnutrition then become rapidly malnourished. So, we saw that a lot.
And we called this out. When my colleagues and I returned from Gaza, we were very vocal about the worrying development of malnutrition. And, of course, all our fears have been realized. Now it’s reached the IPC, you know, Category 5 of malnutrition. There is a famine there. And these are people now, and patients and children, who don’t just need food, they need medical treatment for their malnutrition. And even if there were a ceasefire today, there would be many hundreds, if not thousands, of ongoing deaths from the severe malnutrition as a result of this man-made famine that we’re now seeing.
AMY GOODMAN: Dr. Nick Maynard, what is the prescription you are recommending right now, as you come to this country? You were at the U.N. Now you’re in Washington, speaking to lawmakers. What are you telling them? What do you say that President Biden should do?
DR. NICK MAYNARD: Yeah. We’ve had a terrific reception in New York and in Washington, and we really do believe people are listening to us. And we’re telling them as it is on the ground. We’re not politicians. We’re not lawmakers. We are humanitarians who are just describing the appalling things we have seen.
It is very, very clear to all of us who have been on the ground in Gaza that the only way to try and stop this humanitarian catastrophe is for an immediate ceasefire. There’s a lot of talk back in the U.K. and in the U.S. about how to get aid to Gaza. We can talk about the fact that, undoubtedly, the best way to get aid is over land rather than via airdrops or via sea corridors. But even if they open up the land borders, the crossings, to get the aid in, the distribution of aid within Gaza is virtually impossible with the ongoing military activity. And what is crucial is that aid gets not only to Gaza, but within Gaza easily, to get to all — particularly to northern Gaza, where we know there is now a famine. And so, my message is — our message is that there has to be pressure on the Israelis to stop — and Hamas — to have a ceasefire, so that that aid can be delivered throughout the whole of Gaza and humanitarian care and aid can start to work.
AMY GOODMAN: Well, we know you have to get off to your first meeting today in Washington, D.C. Professor Nick Maynard, surgeon who led an emergency medical team in central Gaza at Al-Aqsa Hospital in December and January, former director for cancer services at Oxford University, thanks so much for being with us.
When we come back, we go to the British Israeli architect Eyal Weizman, the founder of Forensic Architecture. The group’s new report documents how Israel’s attacks on so-called safe zones in Gaza are part of what he calls a “genocidal military campaign.” Back in 20 seconds.











Media Options