
The Food and Drug Administration has recently approved the first drug specifically for African-Americans. The new drug BiDil has raised concerns among some doctors and medical ethicists. We host a debate about this new trend of race-based drug making and marketing. [includes rush transcript]
In June, the Federal Drug Administration approved the drug BiDil to treat heart failure in black patients. It is the first time ever that a medication has been targeted to a specific racial group. On July 5, NitroMed inc., the maker of BiDil, began stocking pharmacies and doctors’ sample closets. It hired 195 new salespeople to begin making calls on 10,000 selected physicians in Philadelphia, Atlanta, New York and Washington and other cities with large African-American populations.
African-Americans suffer from heart failure at almost twice the rate of whites. NitroMed expects BiDil to be prescribed to between 10 and 15 percent of African Americans with congestive heart failure, who number between 250,000 and 750,000 nationwide. But many have criticized this race-based approach to drug making and marketing. They ask how BiDil will affect society’s understanding of the cardiovascular health of African-Americans and whether it will detract from focus on systemic issues like socioeconomic status, residential patterns of segregation, diet and stress from discrimination.
- Dr. Paul Underwood, president of the Association of Black Cardiologists, which was a co-sponsor of the clinical trials for BiDil.
- Jonathan Kahn, law professor at Hamline University. His article “How a Drug Becomes 'Ethnic': Law, Commerce, and the Production of Racial Categories in Medicine,” was published in the Yale Journal of Health Policy, Law, and Ethics last year.
Transcript
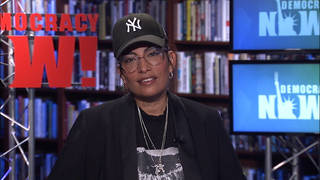
AMY GOODMAN: Joining us on the phone from St. Paul, Minnesota, is Jonathan Kahn. He is a law professor at Hamline University. His article, “How a Drug Becomes 'Ethnic': Law, Commerce, and the Production of Racial Categories in Medicine,” was published in the Yale Journal of Health Policy, Law, and Ethics last year. We are also joined on the telephone by Dr. Paul Underwood, President of the Association of Black Cardiologists. The organization was a co-sponsor of the clinical trials for BiDil. Well, let’s begin with Dr. Underwood. Can you talk about what BiDil is and why it has been approved just for African Americans?
DR. PAUL UNDERWOOD: Okay, well, thank you very, very much. BiDil is a drug that is used for treating heart failure patients, people who have moderate to moderate-severe heart failure. It’s an adjunctive therapy that’s added on top of the standard therapy that’s used, which would include the ACE-Inhibitors and Beta-Blockers as well as usually diuretics. And it’s a combination product with hydralazine and isosorbide dinitrate or basically nitro glycerine.
The way that the drug was developed is that data was examined initially from some heart failure trials that were performed in the 1970s and 1980s, the veterans heart failure trials. And in that small group of African Americans that were included in the trial, it seemed as if this medicine combination was beneficial. And the African American Heart Failure Trial was then designed to study the use of this drug in African Americans who have heart failure. And lo and behold it did seem to be very effective. Using this data, the sponsor, NitroMed, went to the FDA and asked to get the drug approved for use. I believe that since the drug was really studied and shown to be most beneficial in African Americans, that’s why it was approved for use in African Americans, and thus the first race-based medicine that was approved by the Food and Drug Administration.
AMY GOODMAN: Jonathan Kahn, professor at Hamline University School of Law, what is your problem with the approval of BiDil for African Americans?
PROF. JONATHAN KAHN: Well, I think it is a good thing that BiDil was approved. But as you say, I have a big problem with it having been approved in a race specific manner. There are a couple of issues here. The first thing is is that the trials that were — produced the data that were the basis for the FDA approval, the AHeFT trials, they’re called, were only conducted, as Doctor Underwood said, in African American subjects. So there’s no basis for saying whether BiDil works better or differently in African Americans than anybody else. It was simply done in one group. There was no comparison.
Now, for me, at root, what this does is it sends a very troubling message. And that message is that — the fact of the matter is, most of the drugs out on the market today were tested in populations that were almost exclusively white. But we don’t call them white drugs just because the subject happened to be white. The operating assumption was that for the purposes of drug approval, testing a drug in a white person meant that you were just testing it in a human being.
And I think the same assumption should go for when you’re testing a drug in a predominantly black population. The idea being that just because it was tested in a population that happened to be African American doesn’t mean that it’s not good enough for everybody else. The idea being that a drug tested in a white population is good enough for everybody, a drug tested in a black population should be understood to be good for everybody, as well.
AMY GOODMAN: Dr. Paul Underwood, your response?
DR. PAUL UNDERWOOD: Well, certainly, those statements were very true, that it was only studied in African Americans in the African American Heart Failure Trial. However, this drug combination was used in the Veterans Heart Failure Trial in predominantly white patients and that’s when the first inclination that this drug may be more effective in African Americans became true.
What we have found over time, particularly in looking at heart failure, is that there may be some nuances of an individual’s response, as well as of a drug’s benefit, say, looking at ACE-Inhibitors, they may be effective at — perhaps higher doses may be necessary to treat African Americans. Or perhaps African Americans who were treated with ACE-Inhibitors may actually have more of certain side effects than the white population. And it is only through study with trials, such as AHeFT, that we’re looking at trials of overall individuals that we are able to tease out some of these nuances.
Likewise, I believe that when we look at a trial that’s designed, such as the AHeFT trial, we are able to learn more about certain mechanisms of heart failure, and it could be that the ideology, the cause of heart failure in African Americans and whites is different. And that’s why the drug, the drug’s action is different. And that’s why the drug — the drug’s action is different.
There likely isn’t anything specific about the drug combination, the hydralazine isosorbide dinitrate, that makes it useful in people who have darker skin. But it could be that hypertension, high blood pressure is more of a factor in heart failure in African Americans than is coronary artery disease, which seems to be more commonly associated with heart failure in whites.
PROF. JONATHAN KAHN: Yes, that, I agree with completely.
AMY GOODMAN: Jonathan Kahn.
PROF. JONATHAN KAHN: Oh, sorry, but if that’s the case, I think that’s the way that you design a trial or that’s the way you seek indications based on a medical condition, for instance that hypertension — you know, heart failure with hypertension as a precursor, that’s fine, because plenty of people regardless of race have that condition. Race is a terribly crude surrogate in this regard. And so I ask myself, when you get the very reasonable comments that you just made about the different causes of heart failure, I ask myself why doesn’t a company like NitroMed design a drug trial to test for an actual medical condition rather than something based —–basing it on something like race.
DR. PAUL UNDERWOOD: I think that the VHeFT trial really didn’t show the same benefit, say this trend toward improvement in all hypertensive patients, and it was predominately in the African Americans that this trend for benefit was seen.
PROF. JONATHAN KAHN: Well, but it is important to keep in mind that in the VHeFT trial — not to get sort of overly technical in this, but there were only 49 African Americans actually on the BiDil combination in that trial. And in discussing the trial, what happened in the story of BiDil is, it did come for FDA approval in 1996. It was brought to the FDA for approval initially as a drug to treat heart failure in everybody, because some of the same cardiologists who are involved AHeFT believed after these trials in the 1980s, they said, this simply is good to treat heart failure in everybody. And so they brought it to the FDA as a drug to treat heart failure in everybody.
And the FDA did not approve the application at that point, but they didn’t approve it, because they didn’t find that it didn’t work. What they found is that the statistics were too much of a muddle. You know, it’s very technical questions, but they just said, we can’t tell whether it works or not based on these statistics and, in fact, most of the cardiologists on the FDA review panel were saying, we give this drug to our heart failure patients regardless of race, we just give it to them because we all think it works; clinically we believe it works. Back in the 1990s they were saying this. But just the statistics you have given us aren’t good enough for approval. So go back to the drawing board, do a follow-up trial, and we’ll think of it again.
So then it comes back to, why design a follow-up trial based on race? And this is a critical component here because it’s important to understand as a background to all of this the commercial imperatives involved in shaping the science. There are two key patents to BiDil that NitroMed, the corporate sponsor, holds: One is a patent to use the drug to treat heart failure in people regardless of race. That patent expires in two years, in 2007. But in the year 2000, they got a second patent, which was essentially the same as the first patent, but it said, this drug will be used to treat heart failure in–and then they add on–an African American patient. That patent extends until the year 2020. And so it provides an incredible incentive to design a trial that is not looking at, say, hypertension as a precursor to heart failure, but to design a drug that will get FDA approval in a race-specific manner in order to protect their patent rights, not in order to get the best indications for the science, and that’s one of my deep concerns here.
DR. PAUL UNDERWOOD: Well certainly I am —
AMY GOODMAN: Dr. Underwood.
DR. PAUL UNDERWOOD: — what drives NitroMed in seeking the patent applications is something that’s a little bit away from how we view treating patients as a cardiologist. Now the combination of the hydralazine isosorbide dinitrate has actually been approved and is on the guidelines for use in those people and all people who have heart failure, particularly if they are intolerant of the ACE-Inhibitors. So that combination has certainly been in use since the mid 1980s and standard — and it is considered part of standard therapy although it’s not quite as effective as an ACE-Inhibitor. It is used in treating patients who are intolerant of ACE-Inhibitors. The use of the race-specific — or the indication for the patent for African Americans is certainly one that the sponsor, NitroMed, chose based on looking at the data and anticipating the results of the African American Heart Failure Trial.
AMY GOODMAN: Jonathan Kahn of Hamline University.
PROF. JONATHAN KAHN: Well, I basically agree, but then I think, again, in terms of why seeking the race-specific indication when, you know, everybody on the AHeFT trial, everybody involved, all the cardiologists involved in this, all say, of course this drug will work in non-African American people. Nobody makes the claim it won’t work in non-African Americans. There is a potential that it might work in a higher proportion of self-identified African Americans than in self-identified Caucasian Americans but probably for the reason that you say, that African Americans have more hypertension than whites do, things of that sort. But nobody says this will only work in blacks.
And so, the question is why not get it out to everybody? And for me, the only answer I see there is because of trying to make more money off of the drug. And, of course, drug companies, you know, they make money. There’s always a balance between commerce and science in developing drugs. That’s how our system works. I just feel in the case of BiDil, the balance has gotten way out of whack to the point where it is actually skewing the science and sending these very unfortunate and potentially dangerous messages about African Americans being sort of genetically different from other people, which is just wrong. And that’s my broader concern about this. I think it’s great the drug is on the market, but the way it has come on to the market has a lot of very troubling implications.
AMY GOODMAN: Dr. Underwood?
DR. PAUL UNDERWOOD: Well, I think there’s no implication at all that genetics has anything to do with BiDil’s mechanism of action. In fact, there’s no claim that there’s genetics at all. I believe that race in the United States is a social construct, not really a genetic construct. And even though I believe that they’re looking at some genetic data, that data hasn’t been released or analyzed. This is really just looking at a group of individuals who seem to have a higher propensity toward heart failure and more severe ramifications of heart failure. And certainly if a drug is effective in treating this group that has a higher death rate and seems to have a higher prevalence of heart failure, then likely it would be useful in treating the general population, as well. And it’s fortunate that we would have the opportunity to use the drug and perhaps learn more about some of the nuances of heart failure, and perhaps even looking at ideology, such as hypertension versus coronary artery disease, that we will perhaps learn more and be more effective in treating patients and perhaps the drug will be indicated in the future for a larger population. Certainly, I think that it would be in the manufacturer, NitroMed’s best interest to try to open up the indications so that it could be used in all individuals who have heart failure.
AMY GOODMAN: Finally, Jonathan Kahn, NitroMed will make a lot of money combining two generics, the two generics that make up BiDil.
PROF. JONATHAN KAHN: Yes well, it is again important to keep in mind that these two drugs, as you say, are generics that have been on the market for decades. It is estimated that they cost — a combined form of the generics would cost about $0.25 to $0.30 a dose. NitroMed has just priced this drug at $1.80 a dose. That’s about a seven-fold increase over the generics. And so they have priced this not as a matter of how much us costs them to bring to the market, but how much they think the market will bear — how much they will be able to get from insurance companies, and they therefore have also placed it out of the reach of anybody with heart failure who doesn’t happen to be African American, because while they might be able to get a prescription for it, they won’t be able to get their insurance companies to cover it.
AMY GOODMAN: Well, on that note we are going to move on to our next segment, which is related, but we will continue to look at this story. I want to thank Jonathan Kahn, Professor of Law at Hamline University in St. Paul, and Dr. Paul Underwood, President of the Association of Black Cardiologists. Thank you both for joining us.











Media Options