
Guests
- Kelly Posner Gerstenhaberprofessor of psychiatry at Columbia University and the founder and director of The Columbia Lighthouse Project.
Extended web-only conversation with Kelly Posner Gerstenhaber, professor of psychiatry at Columbia University, founder and director of The Columbia Lighthouse Project.
Transcript
AMY GOODMAN: This is Democracy Now!, democracynow.org, The War and Peace Report. I’m Amy Goodman, with Juan González, with Part 2 of our conversation about suicide as a public health crisis in this country.
JUAN GONZÁLEZ: Well, the father of a 6-year-old girl who was killed in the 2012 mass shooting at Sandy Hook Elementary School was found dead by apparent suicide Monday. Jeremy Richman was a neuroscientist who, after the death of his daughter Avielle, founded the Avielle Foundation to support brain science research, with the ultimate goal of preventing violence and building compassion. This is Jeremy Richman speaking just a couple of months after the death of his daughter Avielle.
JEREMY RICHMAN: Another thing that we experience every day is people saying, “I can’t imagine what you’re going through. I can’t imagine what you’re feeling.” But the truth is, anybody that’s cared for somebody else, that loves somebody else, really can imagine what we’re going through. And they should imagine what we’re going through, so that we can change things and prevent senseless violence like this from happening again.
AMY GOODMAN: Jeremy Richman’s death follows two apparent suicides in the last week by survivors of the Parkland massacre. An unnamed student who survived last year’s mass shooting at Marjory Stoneman Douglas High School died by suicide Saturday, and 19-year-old Sydney Aiello, a former student and survivor from Parkland, died the previous weekend. Aiello suffered from post-traumatic stress disorder and, her mother said, survivor’s guilt. Seventeen students, staff and teachers were killed in Parkland on February 14, 2018, in one of the deadliest school shootings in U.S. history.
Our guest right now is Dr. Kelly Posner Gerstenhaber. She’s a professor of psychiatry at Columbia University, founder and director of The Columbia Lighthouse Project, one of the authors of the Columbia Protocol.
What Jeremy Richman said—and this is just so utterly painful that he has taken his own life—said, “Yes, you can imagine what we’re going through.” Can you respond to this?
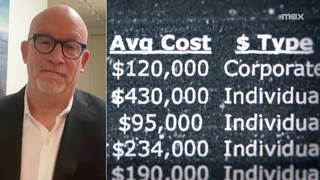
KELLY POSNER GERSTENHABER: Well, I think it really brings home the point that we need to care for the caretakers. We need to screen everybody. You know, suicide, there’s nobody that’s not touched. Takes more firemen than fire, more police than crime, more soldiers than combat. Did you know that if you take a large corporation of 100,000 employees, every six days an employee or a family member will die by suicide. So we need to be asking everybody and screening, so we can connect everybody to the care that they need. You know, police are not only using the Columbia Protocol, for example, to help identify people who need help or need to be taken to the hospital, but also to save their own lives, just like every father and every community member and every person when they get a check-up at the EAP needs to.
AMY GOODMAN: Repeat the questions.
KELLY POSNER GERSTENHABER: Yes. Have you wished you were dead, or have you actually had thoughts of killing yourself? And if that’s yes, have you thought about how you might do this? Have you had these thoughts and had some intention of acting on them? Or have you started to work out or worked out the details of how to kill yourself? And then, have you started to do anything, prepared to do anything to end your life? Which gets at all the things that we have to figure out, if somebody wrote a note, if they collected pills.
And it’s another example of how it relates to prevention of gun violence, as well, very, very poignant, illustrative example. So, 90 percent of shooters have suicidal issues. So we’ve been saying for a long time, let’s ask a few questions and find people who need help before it’s too late. The last shooter that was in Texas, all the way back to Dylan Klebold at Columbine, they wrote notes. They wrote in journals. So, perhaps, if somebody had asked these questions, we might have averted some tragedies, which is what Ryan Petty said to me when we found each other last year. This is the missing link.
AMY GOODMAN: Ryan Petty of Parkland.
KELLY POSNER GERSTENHABER: Yes, the dad who tragically lost his daughter. She was one of the 17 that lost their lives. And he said, you know, the early identification, this is what we need to do. President Obama’s Deputy Secretary of Education Jim Shelton said this years ago. These questions can keep our—help keep our 64 million children safe. And how do we get it in everybody’s hands?
JUAN GONZÁLEZ: We can see a family member asking these questions—a parent or a sister or brother. Now we’re talking—you mentioned large companies. What do you do in the workplace when you see a co-worker, or, if you’re a student, a fellow student at a university, and you’re seeing that some things are not making sense? What would you suggest doing then?
KELLY POSNER GERSTENHABER: Just take out the questions and ask. People will never mind being asked. But they will—they will lose something if you don’t ask. You know, people who are suffering want help.
AMY GOODMAN: But then what do you do?
KELLY POSNER GERSTENHABER: You connect—
AMY GOODMAN: So, it’s someone you might know very well or someone you might not so well—not so well that you care about. What do you do once they say, “Yes, I have considered suicide”?
KELLY POSNER GERSTENHABER: Well, that’s one of the very helpful things about the Columbia Protocol. It’s the first time that we know what questions indicate who’s at imminent risk, the very few people who actually need a next step. And on every Columbia questions or card, it has those next steps. So, if they get those 1 percent high-risk answers, like somebody says, “I have some intention of acting on these thoughts,” or “I collected pills,” then whatever that setting is, you call the crisis line, you walk them to the chaplain, you walk them to the counselor, you know that you have a next step.
AMY GOODMAN: You talk about depression as a major cause.
KELLY POSNER GERSTENHABER: Yes.
AMY GOODMAN: What are signs of depression?
KELLY POSNER GERSTENHABER: Yeah, so, some of the main signs for depression are sad or irritable mood, you know, much of the time something we call anhedonia, which is loss of interest or pleasure. They just don’t enjoy things the way they used to, or they don’t have as much interest in those things. Appetite difficulty, sleep difficulty, concentration difficulty, feeling that—feeling you’re worthless, feelings of guilt, suicidal thoughts. And you don’t have to have all those things, just a number of them together. So people just don’t look the same, and they’re more withdrawn, and they may seem more irritable.
AMY GOODMAN: You know, when someone is suffering—well, let’s say someone breaks their leg. You can say, “Go over to the urgent care center around the corner.” We all see these urgent care centers everywhere. Where do you say go if someone is suffering psychologically, mentally, emotionally?
KELLY POSNER GERSTENHABER: Any medical facility. Any—
AMY GOODMAN: Could you say urgent care?
KELLY POSNER GERSTENHABER: Absolutely, absolutely. So you can take them to the emergency department. You can take them to a clinic nearby. You can call the crisis line, whose number you have up on the—you know, gave earlier. So, there are many resources that—and, by the way, there’s a Columbia app now that you can get in the app store. And it connects to crisis resources. And actually local communities will connect it to their own resources. So, there are lots of, lots of places to get care. And the most important thing is, when you have those high-risk answers, it just means somebody needs a further evaluation, to figure out how—what they need.
AMY GOODMAN: Can you talk about veterans?
KELLY POSNER GERSTENHABER: Yes, yes. So, you know, in the veteran community, we lose 20 veterans a day. But as I said, this is a problem of humanity, right? A hundred and sixteen people die by suicide. And in veterans, the risk is—
AMY GOODMAN: A hundred and sixteen people die?
KELLY POSNER GERSTENHABER: Approximately, per day.
AMY GOODMAN: In the United States?
JUAN GONZÁLEZ: Worldwide?
KELLY POSNER GERSTENHABER: Yes.
JUAN GONZÁLEZ: In the U.S. or worldwide?
KELLY POSNER GERSTENHABER: Yes, yes, in the United States. Yeah. Every 40 seconds across the globe, you know, somebody dies. So, it’s the same kind of problem everywhere. But veterans are certainly at even more increased risk. And what we know—and I work with the Department of Defense and the veterans, you know, very, very closely. And same thing. We know we need to screen. We know we need to ask.
But they were the first ones, the VA and the DOD, to recognize how we’re going to find people and connect them to care. You know, the under secretary of defense wrote an urgent memo that we must go beyond the doctor’s office with the Columbia. We have to find people where they live. And guess what. The Marines were the first ones to test that. They put it in everybody’s hands—clergy, legal assistants, financial aid counselors. It helped them achieve a 22 percent reduction in the rate of suicide that year.
AMY GOODMAN: This is the questions—
KELLY POSNER GERSTENHABER: The questions.
AMY GOODMAN: —to ask, on a card.
KELLY POSNER GERSTENHABER: Exactly. In the Air Force, every airman has it, every spouse, every dentist. Guess what. They were the only service this year to have reductions in suicide. I just went—we’re talking about finding people where they live. I was just at the VA putting these [questions] in the [hands] of every attorney and every community partner across the VA. This is how we’re going to continue to save lives: by equipping every member of the community.
Do you know—you know what really brought it home? I went to give a talk to Connecticut, and this huge system said, “You know, we train the janitors.” And this clinician from the VA said, “Exactly right. I’ll never forget that case where the only person that vet spoke to was the janitor.” And it doesn’t mean he’s ever going to need to ask these questions, but if he’s in a position where it would be helpful, he will be prepared to.
JUAN GONZÁLEZ: And is it your sense that the proliferation of guns has had—made it easier for people to commit suicide or not?
KELLY POSNER GERSTENHABER: Well, I think we have to address every, every method that ends people’s lives, right? And we do know that two-thirds of gun deaths are suicide. And what I always say is, the person who goes to that gun shop to buy that gun to end his life does not want to die, does not know there’s help. That’s why we’re working with the gun community to actually give these questions to the gun shop worker, who, by the way, does not want to sell that gun to the person who’s going to hurt himself or anybody else. Put up posters in gun shops, so that, again, we can let people know that there is help, suicide is preventable, and there are treatments. But we must, must identify the people who need that help.
AMY GOODMAN: And what about kids feeling that even to go to a therapist, well, it still has a stigma, so they’re going to say, “I’m not going to go talk to someone”?
KELLY POSNER GERSTENHABER: It does have a stigma. And the more we can have this conversation, where we normalize and we talk about screening for this like blood pressure or vision testing—and if you had asthma, you would certainly have an inhaler. And this is no different than any other brain-based illness. And we’re making some progress. You know, much of the nation actually sees mental health like any other kind of physical health. But we need to keep breaking down those barriers of stigma, that, as I said, are the major impediment to preventing people from getting the care that they need.
JUAN GONZÁLEZ: And I asked earlier about this, but we didn’t really get a chance to discuss it. The insurance companies—is it your sense that the insurance companies are keeping up with the reality of how they must expand their coverage to assure that people can get the kind of help they need?
KELLY POSNER GERSTENHABER: Yes, and actually see it just the way we’re talking about it, like any other medical illness. So the good news is the Columbia Protocol has been top-down policy in all 50 states and many countries. So, many states, you can’t get Medicaid reimbursement. Insurance companies were the first ones to come and say, “We need to do this. And we need to help people by monitoring in this way.” So, yes, I think they see it this way. We just need to figure out what the barriers are to connect people to the care that they need, once we’ve identified whether they’re at risk.
AMY GOODMAN: How can schools prevent suicide?
KELLY POSNER GERSTENHABER: Well, the first thing they can do is screen and ask. So, every teacher, every cafeteria worker, every student should have the questions to help figure out who needs to be connected to care. And again, also reinforcing all the community resources, all the access to mental healthcare. And after incidents like this, you know, peer-driven and community-driven efforts for identification and treatment are really, really empowering.
AMY GOODMAN: Well, we want to thank you so much for being with us, Dr. Kelly Posner Gerstenhaber, professor of psychiatry at Columbia University, founder and director of The Columbia Lighthouse Project. We’ll link to your piece in the Miami Herald headlined “To help prevent suicide, all we have to do is ask.”
And if people want to get these Columbia Protocol cards, where can they go?
KELLY POSNER GERSTENHABER: The first thing we need to do is ask. So, they can go to cssrs.columbia.edu. And lots of resources, and we’re here to help any community.
AMY GOODMAN: To see Part 1 of our discussion, you can go to democracynow.org. I’m Amy Goodman, with Juan González.










Media Options