
Guests
- Annie Waldmanreporter at ProPublica and author of “How Hospitals Are Failing Black Mothers.” The piece is part of a larger year-long ProPublica investigation, “Lost Mothers: Maternal Care and Preventable Deaths.”
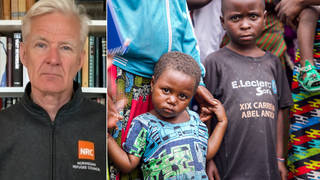
In Harlem, hundreds of people attended the funeral Monday of anti-police brutality activist Erica Garner, who died at the age of 27 on December 30 after an asthma-induced heart attack, four months after giving birth to her second child. Erica’s father, Eric Garner, was killed when police officers in Staten Island wrestled him to the ground, pinned him down and applied a fatal chokehold in 2014. Her funeral came as a new ProPublica investigation suggests Erica Garner’s postpartum death might be part of a wider national problem in which hospitals are failing African-American mothers, leading to disproportionately high maternal mortality rates. Every year in the United States, between 700 and 900 women die from causes related to pregnancy and childbirth. For every woman who dies, dozens more experience severe and sometimes life-threatening complications annually. We speak to Annie Waldman, a reporter at ProPublica. Her most recent article is titled “How Hospitals Are Failing Black Mothers.” The piece is part of a larger year-long ProPublica investigation called “Lost Mothers: Maternal Care and Preventable Deaths.”
Transcript
NERMEEN SHAIKH: In Harlem, hundreds of people attended the funeral Monday of anti-police brutality activist Erica Garner, who died at the age of 27 on December 30th after an asthma-induced heart attack, four months after giving birth to her second child. Erica’s father, Eric Garner, was killed when police officers in Staten Island wrestled him to the ground, pinned him down and applied a fatal chokehold in 2014. Outside the funeral, Shannon Jones of the anti-police brutality organization Why Accountability read from placards about Erica’s death.
SHANNON JONES: [echoed by the People’s Mic] On December 30th, 2017, Erica died after suffering a heart attack. Erica attributed her failing health to the trauma of racial injustice. A new study of mothers in New York City found that black mothers are 12 times more likely to die than white mothers and that racism kills. And that racism kills. Fact five: On August 6, 2017, Erica gave birth to a son, naming him Eric after her father. Erica said, “It’s hard, but you have to keep going, no matter how long it takes. We deserve justice, no matter how long it takes.” We deserve justice, no matter how long it takes! We deserve justice! This is not an isolated incident!
AMY GOODMAN: Shannon Jones of the anti-police brutality group Why Accountability, chanting outside the funeral of Erica Garner, who died just four months after giving birth to her second child, named for her father, Eric Garner.
Well, we turn now to a new ProPublica investigation that suggests Erica Garner’s postpartum death might be part of a wider national problem in which hospitals are failing African-American mothers, leading to disproportionately high maternal mortality rates. Every year in the U.S., between 700 and 900 women die from causes related to pregnancy and childbirth. For every woman who dies, dozens more experience severe and sometimes life-threatening complications annually. Here in New York City, black mothers are 12 times more likely to die than white mothers. That staggering statistic comes from this new investigation by ProPublica.
One new ProPublica article, headlined “How Hospitals Are Failing Black Mothers,” reveals women who deliver at hospitals that disproportionately serve African-American mothers are at a higher risk of danger. The article notes, “[W]hile part of the disparity can be attributed to factors like poverty and inadequate access to health care, there is growing evidence that points to the quality of care at hospitals where a disproportionate number of black women deliver, which are often in neighborhoods disadvantaged by segregation.”
Well, for more, we’re joined by Annie Waldman, reporter at ProPublica who wrote the article, “How Hospitals Are Failing Black Mothers,” the piece part of a larger year-long ProPublica investigation called “Lost Mothers: Maternal Care and Preventable Deaths.”
Annie Waldman, welcome to Democracy Now! We just heard Shannon saying, “This is not an isolated incident.” I mean, you have Eric Garner, his last words, “I can’t breathe,” 11 times, and then his daughter, only a few years later, dying of an asthma-induced heart attack, as she couldn’t breathe, either. Explain what we think, overall, this story may exemplify.
ANNIE WALDMAN: Yeah, well, first I want to say thank you so much for having me here. It’s an honor to speak about this work.
And secondly, you know, when I heard the news of Erica Garner’s death, it was horrifying. It’s incredibly—we, at ProPublica, have spoken to hundreds of women who—and families of mothers who have died in childbirth. And it’s a devastating thing and a heartbreaking thing to lose a mother, a new mother, in childbirth. And in these conversations, the most important thing that seems to come up with African-American women or with white women or women of other races is that it’s an injustice. And it’s injustice because in the United States we have some of the highest rates of maternal death across the board. And most of this is driven by the deaths of black mothers. As we heard in what Shannon was saying earlier, in New York City alone, women are—black women are 12 times more likely to die in childbirth than white women. This is an injustice—an injustice that can be stopped.
NERMEEN SHAIKH: Well, in your piece, as well, or in the ProPublica investigation, I mean, there are some extremely, in addition to what you cited, distressing statistics, that a black woman is 22 percent more likely to die from heart disease than a white women, 71 percent more likely to perish from cervical cancer, but 243 percent more likely to die from pregnancy or childbirth-related causes. The investigation also cites the World Health Organization saying that black expectant and new mothers in the U.S. die at about the same rate as women in countries such as Mexico and Uzbekistan.
ANNIE WALDMAN: Right. And we were trying to understand: Why is this the case? Why is this happening? Why do these rates persist? Even though in the rest of the world the rates of maternal death have actually gone down over the past decade, in the United States the rates of death in childbirth have gone up. And if you actually disaggregate the numbers between black and white women, you’ll see that it’s the number of deaths in the black community which are going up. It’s not just in the white community.
So when we looked at research, we started to ask these questions. You know, researchers have often said it’s poverty, it’s social economic factors, it’s access to healthcare, fragmentation of healthcare. But what we wanted to know was: What can hospitals do? Does it actually—does this disparity persist at the hospital level? Could this actually be something that doctors have some influence on? Could this actually be something where it’s the unconscious bias which is in our healthcare system?
AMY GOODMAN: And what did you find?
ANNIE WALDMAN: We found that definitely that’s the case. If you look at hospitals that disproportionately serve black communities or communities of color, you will find that the number of birth complications are exceptionally higher. And this is not just for birth complications like hemorrhage, which many people see are incredibly preventable—this is not what Erica Garner had—but also when you look at complications such as hypertension disorder, so blood pressure issues, or blood clots, which is something that—I don’t know if you read the Vogue interview with Serena Williams yesterday, but she spoke about her tragic birth complication that she faced.
AMY GOODMAN: This is the tennis star.
ANNIE WALDMAN: The tennis star, the queen of the court. Even she experienced a birth complication at the hands of her doctor. She has a history of blood clots. She has a history of—I think she had a blood clot a couple years ago that took her off of the courts for a year. This is something the doctor should have been aware of when she came into the hospital.
AMY GOODMAN: She self-diagnosed.
ANNIE WALDMAN: She self-diagnosed, exactly. And should women have to go into the hospital and self-diagnose? I mean, there are medical staff for that. And, in fact, in the story, if you read closely, she asked the nurse, in order to get some kind of treatment, in order to get a CT scan, to see if here blood clots were getting worse. And the nurse said, “Oh, it’s the pain medication, which might be confusing you.” I mean, what does this make us feel as women? What would black women feel about this, to know that their pain is being ignored, their symptoms are being ignored? And, in fact, studies have shown that pain management is something—it’s a huge problem in communities of color. Doctors frequently do not give the right pain medication to black women, and they believe that sometimes it might be, like what happened to Serena Williams, somewhat in their head, or they might be confused.
AMY GOODMAN: Can you talk about the stories of Dacheca and Tanesia?
ANNIE WALDMAN: Yeah. So, while we were—how we started with this investigation, at least the one looking into hospitals, was with the data. We wanted to find the hospitals that had the highest rates of birth complications. And what we did was we looked at three states, millions of births, so much data that it would overwhelm you. But what we wanted were the human stories. So we worked with an amazing team at ProPublica that does engagement, and they reached out to communities, asking for stories. Coincidentally, we were investigating one hospital in Brooklyn that had one of the highest rates of maternal harm in New York state, and a family reached out to us and said, “Our mother died there.” This—
AMY GOODMAN: Can you tell us what hospital it is?
ANNIE WALDMAN: Yes. It’s SUNY Downstate in Brooklyn. This is in a triangle that has—in Brooklyn, which is a borough in New York City, which has one of the highest rates of birth complications. One of the neighborhoods just near this hospital, Brownsville, one in 20 women there have a birth complication when they go into a hospital. So, when you think of these numbers, this is not just a rare occurrence. This is an everyday thing for these communities.
So, Dacheca Fleurimond, one of the women that we focused on, she died just months before our investigation into hospitals. We started looking in to her case. She was incredibly—while she was at risk, she had no idea that she was going to die when she walked into the hospital. She had had five previous pregnancies. All of them went fine. She was pregnant with twins. She didn’t know that she was actually at very, very high risk for a blood clot, what Serena Williams also experienced. Thirty-six hours after her cesarean section, she died.
And what was shocking about this, even though this is incredibly devastating just on its own, while we were investigating this hospital, another woman passed away, Tanesia Walker. She was 31 years old, just a few weeks shy of her 32nd birthday. And she was an American Airlines flight attendant. She had a kid before. She had a job. She was financially stable. She had a criminal justice degree from John Jay University here in New York City. She had her life in front of her, just like all of these women. And yet, when she walked into this hospital, she had no idea that within 24 hours she would also die. At this time, we don’t know exactly the cause of her death, but her family believes that it might have been a blood clot, the same thing as Dacheca Fleurimond, the woman who died at the same hospital just months before.
This brings up so many questions of: What are hospitals doing to investigate the deaths that occur on their own grounds? What are doctors doing in order to change the protocols, once a death happens? What is the conversation that happens? You know, I asked the hospital all these questions, and, unfortunately, they did not answer these questions. So I think that it’s really up for the public to put pressure.
AMY GOODMAN: And insurance, what role does that play, and lack of it?
ANNIE WALDMAN: Yeah, I mean, insurance plays a huge role. This is really part of a systemic issue. It’s not just the hospitals. It goes down to, you know, when a child is born and born into this society and whether they have healthcare. And then they grow up, and do they have good education? I mean, this is not just about the segregation of our healthcare system. This is about the segregation of our entire society, from education to housing and onward.
AMY GOODMAN: We want to thank you so much for being with us. This interesting point—it was written in the New York Post: “Pearson, the world’s biggest education company, has come under fire … for a page in one of its nursing textbooks—which features racist stereotypes about minorities,” one line saying, “Blacks often report higher pain intensity than other cultures.” “The harmful misconceptions can be found on page 161 of the textbook, 'Nursing: A Concept-Based Approach to Learning, Volume I.'”
ANNIE WALDMAN: Yeah. So, as you will see, there is unconscious bias and bias in everything that we read, you know, and it’s really time for people to start standing up and questioning what’s happening.
AMY GOODMAN: We want to question you further about this; we’re going to post it online at democracynow.org. So please stay with us. But, for now, we’re going to break and then looking at another aspect of the life of Erica Garner that so many women experience now, as they deal with the stress of losing loved ones to police brutality. This is Democracy Now! Annie Waldman’s pieces and the whole ProPublica series, we’ll link to at democracynow.org, “How Hospitals Are Failing Black Mothers” and more. Stay with us.
[break]
AMY GOODMAN: “Four Women” by Nina Simone. The late Nina Simone, great singer, will be inducted into the Rock and Roll Hall of Fame on April 14th.











Media Options