
Guests
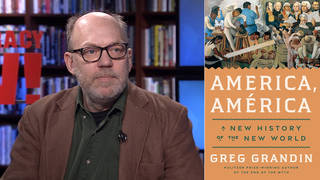
- Annie Waldmanreporter at ProPublica and author of “How Hospitals Are Failing Black Mothers.” The piece is part of a larger year-long ProPublica investigation, “Lost Mothers: Maternal Care and Preventable Deaths.”
In a new article in Vogue, tennis star Serena Williams told the magazine how she self-diagnosed a life-threatening emergency after giving birth. Shortly after delivering, the tennis star suddenly felt out of breath and assumed she was having a pulmonary embolism, given her history of blood clots. According to Vogue, “She walked out of the hospital room so her mother wouldn’t worry and told the nearest nurse, between gasps, that she needed a CT scan with contrast and IV heparin (a blood thinner) right away. The nurse thought her pain medicine might be making her confused. But Serena insisted, and soon enough a doctor was performing an ultrasound of her legs. 'I was like, a Doppler? I told you, I need a CT scan and a heparin drip,' she remembers telling the team. The ultrasound revealed nothing, so they sent her for the CT, and sure enough, several small blood clots had settled in her lungs. Minutes later she was on the drip. 'I was like, listen to Dr. Williams!'” We speak to Annie Waldman, a reporter at ProPublica who wrote the article “How Hospitals Are Failing Black Mothers.” The piece is part of a larger year-long ProPublica investigation called “Lost Mothers: Maternal Care and Preventable Deaths.”
Transcript
AMY GOODMAN: This is Democracy Now!, democracynow.org, The War and Peace Report. I’m Amy Goodman, with Nermeen Shaikh.
NERMEEN SHAIKH: Tennis star Serena Williams and her husband, Reddit co-founder Alexis Ohanian, recently welcomed into the world their daughter, Alexis Olympia Ohanian Jr. The baby was born on September 1st by emergency C-section. Williams recently told Vogue magazine how she self-diagnosed a life-threatening emergency after giving birth. Shortly after delivering, the tennis star suddenly felt out of breath and assumed she was having a pulmonary embolism, given her history of blood clots.
According to Vogue, quote, “She walked out of the hospital room so her mother wouldn’t worry and told the nearest nurse, between gasps, that she needed a CT scan with contrast and IV heparin (a blood thinner) right away. The nurse thought her pain medicine might be making her confused. But Serena insisted, and soon enough a doctor was performing an ultrasound of her legs. 'I was like, a Doppler? I told you, I need a CT scan and a heparin drip,' she remembers telling the team. The ultrasound revealed nothing, so they sent her for the CT, and sure enough, several small blood clots had settled in her lungs. Minutes later she was on the drip. 'I was like, listen to Dr. Williams!'”
While Vogue did not identify the hospital, several news outlets reported St. Mary’s Medical Center in West Palm Beach is the hospital where Serena Williams gave birth.
AMY GOODMAN: What happened to Serena Williams is not an isolated event. Every year in the United States, between 700 and 900 women die from causes related to pregnancy and child birth. For every woman who dies, dozens more experience severe and sometimes life-threatening complications annually. Here in New York City, black mothers are 12 times more likely to die than white mothers. That staggering statistic comes from a new investigation by ProPublica.
For more, we are continuing our conversation with Annie Waldman, in Part 2, a reporter at ProPublica, who wrote the article, “How Hospitals Are Failing Black Mothers.” The article reveals that women who deliver at hospitals that disproportionately serve African-American mothers are at a higher risk of danger. The piece is part of a larger year-long ProPublica investigation called “Lost Mothers: Maternal Care and Preventable Deaths.”
We began, Annie, this segment by talking about Serena Williams. Clearly, you assume, she and her Reddit founder husband are at one of the top hospitals, you would expect.
ANNIE WALDMAN: Right.
AMY GOODMAN: And yet she even is getting inferior care. Can you comment on what happened to her? And then we’ll talk about situations like Erica Garner, who died at the age of 27, the anti-police brutality activist, in New York City, four months after giving birth to her second child.
ANNIE WALDMAN: Certainly. Serena Williams is the queen of the court, one of the world’s greatest athletes, if not the world’s greatest athlete right now. She’s a multimillionaire, along with her husband. Obviously, they have incredible medical coaches for her career, for her—for tennis. But you would assume that she also has one of the greatest doctors who’s working on her as she’s giving birth, who she’s able to see, and can identify that she is a high-risk patient. Serena Williams, a few years ago, had a blood clot, which puts her at a much higher risk of having blood clots during birth. And on top of that, she had an emergency cesarean, which, if you look at ACOG, which is the American College for Gynecologists and Obstetricians, they will even mention that, you know, a cesarean section puts you at higher risk. So, with these risk factors, it’s shocking to me that she went into the hospital, knowing this, felt that she had the symptoms of a pulmonary embolism, told the medical staff around her that she had perhaps a pulmonary embolism, and that they still doubted her, doubted her with all of her experience, doubted her with her intelligence, doubted her with the knowledge of her own body, what she knows best.
And so, this is really emblematic of a much larger problem in this country, where the—black women, their concerns about their health, about pain, about everything that happens to them in a hospital, can sometimes be ignored, and, more broadly, the fact that they have experienced much higher rates of birth complications. And these things are not unconnected. They’re definitely connected. And so, if you see Serena Williams, who is a superstar, and this happens to her, you can only imagine what happens to the multitude of mothers out there who are middle-class, lower-income, who don’t have insurance, who are on Medicaid, who are in inner-city hospitals. Where is their Vogue article? They’re not going to have it, right? So, essentially, what happened to her, she was still ignored. We have to also listen to the experiences and the stories of women who are frequently ignored.
NERMEEN SHAIKH: Well, Annie, in the ProPublica investigation, the investigation revealed that the hospitals with high maternal mortality rates take on patients who have less access to consistent, quality prenatal care—obviously this is not the case with Serena Williams—or have chronic health issues, like diabetes or heart disease, that make pregnancy and childbirth riskier. So, the question there is: Do hospitals need to be reformed? I mean, obviously, from what the investigation finds, they do. But it seems that the problem is much more systemic, of the provision of suitable healthcare.
ANNIE WALDMAN: Right. I mean, it is systemic. And, you know, this was something that we really discussed in our newsroom. For example, you know, black women have higher rates of heart disease. Is this something that contributes to the higher rates of death? Or is it the hospital? Right? But it’s not either/or, it’s actually both. The fact is, is that hospitals are responsible for all women who walk in to their doors. They’re responsible not only for having equal care, but care that suits their needs. This is not about equal standards of care. This is about making sure that high-risk women, regardless of their race, have the medical care that they deserve when they walk in those doors. And if women without health insurance, women on Medicaid, black women are at higher risk of things like pulmonary embolism, diabetes, hypertension, that should be noted when they walk in the doors of a hospital.
AMY GOODMAN: How can you find out the record of a hospital, before you decide where you want to go or, for example, give birth?
ANNIE WALDMAN: That’s a really good question. Researchers have a lot of access to data, so they have really been able to do these analyses and say, “Oh, these hospitals have higher birth complication rates.” We’ve also been able to do that, but that’s only because I’m a computer programmer, and I can actually crunch the data, dive into the numbers and figure out what’s going on. For most women, this information is not out there. And if you look in the studies, most of these hospitals that have high complication rates are unnamed. And so, most of the stories that happen at these hospitals go untold. And what’s important is that we need—you know, I’m a data evangelist. I believe in open data. I believe in transparency of data. And I believe that this information needs to get out there, so that women can make the best choices that they have.
AMY GOODMAN: You name names in the article, in this series, names of hospitals. Can you talk to us about them and the states that you looked at?
ANNIE WALDMAN: Yeah, so, we really focused—we dove into New York City, because in New York City black women are 12 times more likely to die than white women, which is an astronomical statistic. It’s horrifying.
AMY GOODMAN: Can you say that one more time?
ANNIE WALDMAN: Black women are 12 times more likely to die in childbirth than white women. When you hear a statistic like that, it should make you stop in your tracks. You should really be thinking, “Why is that? And why has that not changed?” In fact, this statistic has gotten worse. Just a few years ago, it was eight times more likely to die in childbirth. Today it’s 12. Why is this getting worse?
And so, when we think about these statistics, you know, it’s not enough just to say them. You have to go into the stories. You have to listen to the mothers who have experienced complications. You have to listen to the families who have lost mothers, and try to humanize it so people understand the urgency of this situation.
And most importantly in that is really saying to the hospitals, “What are you doing to improve these numbers?” And importantly in that is calling out some of these hospitals that have incredibly high rates. So, in our investigation that we did, “How Hospitals Are Failing Black Mothers,” we looked at one hospital in Brooklyn, which is SUNY Downstate, and really asked them, “Why do you have such high birth complications?”
And as I mentioned before, in Part 1, while we were investigating this hospital, we heard of a death that occurred three months before our investigation began, and we started looking into that. And then, just a few weeks later, while we were continuing our investigation into the death of this other mother, another mother died at this hospital.
You know, what it says to families, when I show up at their doorstep, just days after they lost somebody who was so critical to the cohesiveness of their family, what it says to these families when I show up and say, “Oh, did you know that three months ago another woman died in childbirth?” it says that, honestly, this—their lives, what do they matter? What do they matter to these hospitals? Are people even investigating this, the fact that these stories aren’t out there, the fact that people aren’t in the streets over mothers dying at hospitals? You know, do their lives matter?
And this is an injustice that can be stopped. There are protocol changes that some hospitals are making in order to increase, you know, the likelihood that women are not going to have a birth complication. With pulmonary embolism, what Serena Williams experienced, she could have taken a blood thinner, especially because she was high-risk. If you go on over to the United Kingdom, all women who have cesareans are on blood thinners. So, Serena Williams would have been on a blood thinner. The women in my story, they probably would have been on a blood thinner, as well, having had cesareans. But we’re not making these changes in all hospitals. And that’s something that we really have to question.
AMY GOODMAN: That’s extremely important, right? Because there’s a very high rate of cesareans performed in the United States, much more so than many other countries.
ANNIE WALDMAN: Exactly. And a lot of people believe that that is what’s driving the high complication rates in the United States. Years ago, you know, a cesarean was a rare thing. It was only done in an emergency. But these days, some hospitals have a third of their women, you know, half of their women having cesareans. Those are astronomical rates when you compare them to other industrialized countries.
AMY GOODMAN: So that you can fit in to a doctor’s schedule, right? They can—
ANNIE WALDMAN: Well, that is what some people say, is that it’s just for scheduling. It makes it easier. On top of that, there have been some studies which have shown that cesareans actually allow hospitals to bill higher, so they’re able to make a little more money off of it. Whether that’s actually what’s driving the rates is questionable, but it’s something that people actually have to think about.
NERMEEN SHAIKH: Well, one of the things that you mentioned in Part 1 is that maternal mortality rates in the rest of the world have been steadily declining.
ANNIE WALDMAN: Right.
NERMEEN SHAIKH: But in the U.S., of course, they’re rising. Could you say a little about how the U.S. compares—I mean, you mentioned a little bit about this now—to other industrialized countries, countries in Europe, not just the U.K., and Japan, and then how it compares? I mean, earlier we talked about comparisons to Mexico and Uzbekistan. I mean, the United States is, of course, one of the richest countries in the world, so this is really quite shocking.
ANNIE WALDMAN: If you look at industrialized countries, I think we’re around 17. So we are at the bottom of the list, even though people love to say about how great America’s healthcare system is. You know, we are at the bottom of the list for mothers. We are failing mothers when it comes to healthcare. And if you look at, you know, other countries, say, Sweden or the United Kingdom, their rights are sometimes a third of what we have. I think our rate right now is about 26 women die per 100,000. In Europe, in Sweden and a lot of these other industrialized countries, it’s underneath nine. We are leagues above other people when it comes to maternal deaths.
And this is something that the United States has been aware of, the CDC has been aware of, the WHO has reported on. These are not statistics which are shocking to those who are experts in this field. But, for whatever reason, these rates are not changing. In fact, they’re increasing. And as we said before in Part 1, a lot of this is driven by the high rates of harm and death in the black community.
AMY GOODMAN: You mentioned the word “protocol.” That may make people’s eyes glaze over. But it’s something you feel is extremely important. Talk about how hospitals are changing their protocols. What does the word even mean?
ANNIE WALDMAN: So, a protocol, essentially, is: When a medical emergency happens, what is the standard operating procedure? What is done first? Is there—you know, what medicine is drawn? Do people have blood waiting to insert it into somebody through an IV? So they’re actual steps that people can take to make sure they respond to these emergencies better.
In California, there’s an incredible expert there, Dr. Elliott Main, who has been developing better protocols, specifically for hemorrhage, which is one of the most preventable causes—preventable causes of birth complications. And what he found was that when he increased the protocols, made the protocols better in the hospitals, 20—birth complications decreased by 20 percent, not just complications related to hemorrhage, but complications across the board.
And what this says is that there are actionable things that hospitals can do. They can take measures that will actually improve the healthcare of women. Yet, hospitals across the United States are not doing this. And whether it’s because of clinging to tradition or believing that their protocols are better than innovative protocols which are coming out of California or other states, who knows?
But a lot of it stems down to the fact that we need to listen to black mothers more. We need to listen to their stories. We need to listen what’s happening to them and take this seriously and start thinking about how we can not just serve the entire population, but how we can serve people at high risk, which is black mothers.
AMY GOODMAN: So, what are mothers’ rights when they go into a hospital? I was with a friend who was giving birth at a hospital here in New York, one of the finest. And one of the things that the doctor said to her, when she said she wanted to keep trying before having a cesarean or before getting drugs, just to keep on—give her a little time, he said he might be on another floor, and she would be risking a lot. What if he had to deal with another emergency when she finally, you know, was—t was time for her to give birth? And so, if she took the drugs right then, he would be right there. That’s what he could guarantee. This is one of the top hospitals in New York.
ANNIE WALDMAN: A woman who’s in childbirth should not have to make that decision right then and there. That’s a tragedy. I’m really sorry for your friend. I mean, women, when they give birth, can go to any hospital that they want. They can take a taxi. They can go anywhere. But when an ambulance comes to your doorstep and you’re in labor, they will take you to the nearest hospital, which means that women who are in areas which have been segregated for years are going to go to some of those hospitals, which have some of the highest complication rates. Once they get there, they can argue—
AMY GOODMAN: Can you tell an ambulance that’s connected to a particular hospital, “I don’t want to go there. I want to go to this other hospital”?
ANNIE WALDMAN: You can tell an ambulance that, but whether they will take you to that other hospital is between you and the person who’s driving that ambulance. I spoke with many women who said—
AMY GOODMAN: So, are you saying a pregnant woman who’s about to give birth has to commandeer the ambulance and drive it herself?
ANNIE WALDMAN: It seems like it. It’s tragic that that might actually be the case. But, you know, I spoke with many women who begged ambulance drivers to take them to other hospitals, sometimes hospitals where they had all of their prenatal care, because they were trying to get out of the nearest hospitals to them, which had some high rates or they had heard negative things about. And so, they still weren’t able to go to the hospital where their prenatal care was. They had to go to the nearest hospital.
And, you know, once women arrive at the hospital, they can advocate for themselves, they can say that they don’t want a cesarean, but sometimes it’s really hard, in the face of medical care, to stand up to a doctor and say, “I know my body. I know what’s best for me.” And when it comes to communities which have low resources, which don’t have a lot of necessarily medical education for women in the community, it can be really difficult to stand up to a doctor who’s telling you, “You might die if you don’t have the cesarean section.”
And this trickles down. You know, the first cesarean, the complication rates are quite low. But for every child after that, if you—you are required to have a cesarean pretty much all the time after each cesarean, and the complication rates increase. So it’s not necessarily that first childbirth that you might face a complication, but it sets you up for problems way down the road.
NERMEEN SHAIKH: And are you familiar with the hospital, Woodhull Hospital in Brooklyn, where Erica Garner, in fact, gave birth, and then, herself, four months later, died?
ANNIE WALDMAN: Yeah. And to be honest, it is one of the hospitals that we looked at. It does have one of the higher rates of birth complications in the city. But New York City Health + Hospitals Corporation, which runs all the public hospitals in New York City, had a lengthy conversation with me, and they have a lot of protocols that they’re changing. They’re aware that this is something that’s important. They’re aware that many of the patients who come to their hospital, particularly mothers, are at higher risk. And they are trying to put these new protocols in place. So, even though some of their rates, on paper, right now may seem a little bit higher, they are proud of the steps that they are taking to change. That was not the case with every hospital that we looked at and not the case with every hospital where we found deaths of mothers.
AMY GOODMAN: Where was the most egregious—what were the most egregious hospitals?
ANNIE WALDMAN: I would have to say the hospital that we really focused on, which was SUNY Downstate. I mean—
AMY GOODMAN: And what’s amazing about this, for people outside of New York, when you say SUNY Downstate, SUNY is the State University—
ANNIE WALDMAN: Exactly.
AMY GOODMAN: —of New York. It’s a teaching hospital. It’s linked to the State University system.
ANNIE WALDMAN: Right. And this is something that the state is responsible for. So there are city hospitals in New York City, but this one is actually organized and run by the state. And if you—it has had a bumpy history. It has faced bankruptcy, fears of bankruptcy a number of times. But it also has faced some allegations of mismanagement, especially when it comes to its finances. So, you know, what goes on behind the closed doors, it’s hard to say, but what’s clear is that low resources is not an excuse. It can’t be an excuse for some of these hospitals, because there are some hospitals with low resources which are doing well and trying to change their protocols. What’s happening at SUNY Downstate, it’s really hard to say.
But what’s shocking to me, again, going back to this, is that when you keep hearing of the deaths of women at these hospitals, and you know that these complications are preventable—60 percent, around 60 percent, of birth complications are preventable—you have to ask: What’s going on? Why are some hospitals worse than others? Why are your rates of risk higher at some hospitals than others?
AMY GOODMAN: Finally, Annie, what most surprised you? And what are you going to pursue looking at now?
ANNIE WALDMAN: I think what most surprised me was that—when we started publishing these stories about a year ago, what surprised me was how this reverberated across all communities, across all women. You know, we weren’t sure that people would really read these stories, but there has been an enormous feedback about this. And a lot of women want to share these stories.
And I think that that’s the most important thing. I don’t want to sit up here and speak for all black women. I can’t. But what I can say is that it’s important to listen to black women. It’s important to listen to all women about the complications that they’ve experienced, because once these stories get out there, like what happened to Serena Williams, once survivors start talking about what happened to them, that’s when real change can happen.
AMY GOODMAN: Well, I want to thank you very much for being with us and being with us after the death of Erica Garner. Again, while people knew her as a remarkable young activist who has been fighting for justice for the death of her father, who died in a police chokehold, oh, several years ago, Eric Garner, she herself died, taking her last gasps in an asthma-induced heart attack, four months after she gave birth to her second child, a little boy, who she named after her father, a little boy named Eric. Annie Waldman, thanks so much for being with us, reporter at ProPublica, where her most recent article is headlined “How Hospitals Are Failing Black Mothers,” part of a larger year-long series called “Lost Mothers: Maternal Care and Preventable Deaths.” We’ll link to the whole series at democracynow.org.
And to see Part 1 of our conversation with Annie Waldman, go to democracynow.org. I’m Amy Goodman, with Nermeen Shaikh. Thanks so much for joining us.








Media Options