
Guests
- Paul Farmerinfectious diseases doctor and medical anthropologist. He is a professor of medicine at Harvard University, chair of global health and social medicine at Harvard Medical School, co-founder and chief strategist of Partners in Health.
As the United States sets records for COVID-19 deaths and hospitalizations, we speak with one of the world’s leading experts on infectious diseases, Dr. Paul Farmer, who says the devastating death toll in the U.S. reflects decades of underinvestment in public health and centuries of social inequality. “All the social pathologies of our nation come to the fore during epidemics,” says Dr. Farmer, a professor of medicine at Harvard University, chair of global health and social medicine at Harvard Medical School and co-founder and chief strategist of Partners in Health.
Transcript
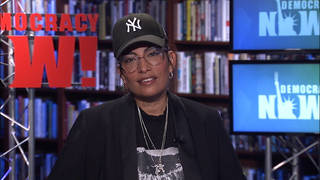
AMY GOODMAN: This is Democracy Now!, democracynow.org, The Quarantine Report. I’m Amy Goodman.
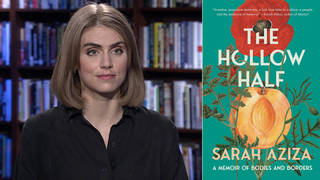
As we continue our coverage of the COVID-19 crisis, we turn now to the world-renowned infectious disease doctor and medical anthropologist, Dr. Paul Farmer. He’s chair of global health and social medicine at Harvard Medical School and co-founder of Partners in Health, an international nonprofit that provides direct healthcare services to those who are sick and living in poverty around the world. Dr. Farmer co-founded the group in 1987 to deliver healthcare to people in Haiti. In 2014, Partners in Health was one of the first organizations to respond to the Ebola crisis in West Africa. Dr. Farmer’s new book is titled Fevers, Feuds, and Diamonds: Ebola and the Ravages of History. I spoke to him in early December and asked him how it’s possible for the United States to have nearly 20% of the world’s infections and deaths while having less than 5% of the world’s population.
DR. PAUL FARMER: Well, I mean, we are facing the consequences of decades and decades of underinvestment in public health and of centuries of misallocation of funds away from those who need that help most. And, you know, all the social pathologies of our nation come to the fore during epidemics. And during a pandemic like this one, we’re going to be showing the rest of the world, warts and all, how — we have shown the rest of the world how badly we can do. And now we have to rally, use new tools that are coming online, but address some of the older pathologies of our care delivery system and of our country. I think that’s where we are right now.
AMY GOODMAN: What needs to happen right now in the United States?
DR. PAUL FARMER: Well, first of all, you know, I think that it’s a great tragedy that such matters as masking or social distancing or even shutting down parts of the economy, that contribute to risk but are — it’s just a shame that that’s been politicized. These are not political or partisan actions. They are public health strategies. Right now they’re all we’ve got.
But even when the vaccine is online or begins to come online, we have no history of seeing a vaccine taken up so rapidly that it would alter the fundamental dynamics of a respiratory illness like this. So, we’re facing, as President-elect Biden said, a long, dark winter. And if we can make a difference that could spare tens of thousands and perhaps more than 150,000 lives, then we should do that.
And whether or not these are called mask mandates or pleading from the president, we need state and local authorities to come together and underline the nonpartisan and life-saving nature of some of these basic protective measures. We need to invest very heavily in making sure the vaccine goes to those who need it most and those who have been shut out of previous developments like this or shut out for too long.
So we have a lot of work ahead of us this winter, but no small amount of it is going to rely on individual families and communities to take up some of these measures rapidly to make sure that the dark winter does not lead to a blighted spring.
AMY GOODMAN: Dr. Farmer, can you comment quickly on these vaccines, for people to understand, the first what’s called mRNA, messenger RNA, vaccines, what they actually do in the human body? Do they make you immune, or you can get sick and be a carrier, but you, yourself — I mean, you can be infected and be a carrier, but you, yourself, will not get very sick? Explain the choice of who gets the vaccine, also the fact that this has not been studied in children, people under 14, and so what this means for kids.
DR. PAUL FARMER: Well, in general terms, let me just say that in the 30-plus years I’ve been involved in this work, I’ve never seen such a rapid development of a novel preventive for a novel vaccine. So there’s a lot to celebrate in terms of the global effort to come together to develop new vaccines.
Again in general terms, the idea is that instead of having a natural infection — in this case, breathing in the novel coronavirus and getting sick, which leads to the outcomes that we know: death or recovery with sequelae — it also leads probably to immunity. That’s what it’s like with other viral infections in humans, or almost all of them. So, what the vaccine does is introduce something that will trick the body into believing that it’s being invaded by the virus — in this case, it’s focused on a particular protein on the outer surface of the virus — and generate that immune response, which is often robust and enduring, at least with other viruses. Now, in the case of any novel pathogen, we don’t know for sure how long that immunity lasts, right? I mean, how could you? It hasn’t been studied for long. But we know about other viruses and can take some lessons from those.
And in the case of this new vaccine or this new type of vaccines, the mRNA vaccine, we’re also dealing with that unknown. This is a new kind of vaccination. This is a new approach. It’s very exciting, in part because it seems to confer that immunity without significant adverse effects. So, I think, again, on the side of development of a novel technology, these vaccines, whether mRNA vaccines or others, are great news, right? And maybe they will influence a new generation of vaccines for other pathogens, particularly viral pathogens, which tend to be the worst ones among humans. So, that’s where we are with the development of new technology.
Unfortunately, as I said and as you’ve underlined many times, Amy, the old pathologies of our society make it unlikely that the rollout will be smooth and evenly taken up across various communities, some of them with well-founded fears and mistrust of any kind of public health campaign. So, we’re in a bit of a pickle. I’m optimistic about what will happen in this country, but as you pointed out in opening up the hour, a lot of us are concerned with what’s going to happen in the Global South and among those who might as well be considered living in the Global South in wealthy and egalitarian countries like the United States and parts of Europe.
So, it’s going to be a rocky winter, with some highs and lows. And I hope there are more highs than lows. I hope there’s more reason for celebration than for grief. But I think it’s going to be a very, very difficult winter.
AMY GOODMAN: Just before we go to this remarkable book about dealing with Ebola and what it meant, I wanted to ask you about property rights, about patents and about countries like South Africa and India pushing for a temporary suspension of intellectual property rights and patents so that COVID-19 vaccines and medications become more accessible, particularly in the Global South.
DR. PAUL FARMER: Well, I’d just like to say something we’ve had a chance to discuss before in previous years. You know, when you look at what happened around HIV, which by 1995, '96, those of us in the infectious disease world understood that this would be a life-saving suppressive therapy — like as with diabetes requiring insulin, you'd have to keep taking it, but this would save millions of lives, and maybe even more, and prevent transmission of mother to child — the same debates about intellectual property of course came up then.
The average wholesale price for a three-drug regimen in the years immediately after the discovery of these new agents was $15,000, sometimes $20,000, per person per year. So, if you split your time between Harvard and Haiti, as I had and do, you would imagine, if you couldn’t have an imagination beyond conventional property rights discussion, that the majority of the world would be shut out of access to this therapy. And, of course, that made the most difference, on a continent level, in Africa, where the majority of people living with HIV and dying with HIV were at the time.
And what happened later was the production of generic versions of these drugs, often in India or China or even South Africa — right? — so that a much lower cost could be tied to the same agents. And when I say “much lower,” I mean a reduction, really even within those early years, from $15,000 to $20,000, to about $300 per person per year. And with groups like the Clinton Foundation getting involved, those prices dropped even further. And right now you can get a really good three-drug regimen, even with some pediatric formulations for children, for about $60 per patient per year.
So, you could say that took a long time, but it didn’t take a long time in terms of the impact that it could have. Millions and millions of lives, maybe even 16 to 20 million lives, are being saved by these drugs. But in some places, like Rwanda, where I’ve spent 10 years, you saw the virtual eradication of AIDS among children, because if mom is on therapy, the transmission to babies in utero, or through breastfeeding probably, really does not occur. And this is not a hypothetical development. This has already happened in Rwanda, which is a very poor country with a very robust public health and care delivery system.
AMY GOODMAN: Dr. Paul Farmer. We’ll return to our interview in a moment and talk about his new book, Fevers, Feuds, and Diamonds: Ebola and the Ravages of History.










Media Options